If you thought the answer is “the low FODMAP diet”, you wouldn’t be the only one. Sadly, it’s not as simple as you might expect.
As a dietitian, I’ve taken care of a lot of different kinds of people with all kinds of health problems. Everyone is an individual and diet must always be individualized, but it seems that IBS is much more difficult to generalize than other health problems.
For example, if you have diabetes, you should always pay attention to everything that affects your blood sugar levels. Most often this means counting all the carbohydrates you eat, and sometimes also taking protein and fat into account. For cardiovascular disease, fat quality is something that everyone with high cholesterol needs to consider.

When it comes to IBS, there is no “one-size-fits-all” diet that works for everyone. For one, there are four different IBS types and the advice you give to someone with diarrhea is not the same if the problem is constipation instead.
While the low FODMAP diet is the most “popular” diet for IBS, in my expert opinion, the low FODMAP diet is overused and is NOT a good idea for many, if not most, people. You can read why in my two blog posts “Is the low FODMAP diet the best diet for IBS?” and “Should you try the low FODMAP diet for IBS?”. I know most other dietitians love the low FODMAP diet, but I can’t overlook all the problems that come with this diet. Yes, FODMAPs are small fibers that are easily fermented by your gut microbes and cause relatively more gas, but this happens in everyone, not just in people with IBS. The reason why you are more sensitive to them is because of visceral hypersensitivity, which is caused by IBS (this sensitivity is something I want to improve, rather than just remove foods as a bandaid solution).
So, if it’s not the low FODMAP diet, then what is the right diet for IBS?
It certainly is a highly individualized one. Here are the first five diet and food related questions you should ask yourself regardless of your IBS symptoms:
- How often do I eat?
- How big are my meals?
- How quickly do I eat?
- Do I chew my food until it’s apple sauce consistency?
- What’s my frame of mind when I eat?

I find that regular eating times, and not eating too often or too seldom, lay a foundation for a gut healthy diet. This way you are less likely to overeat or keep taxing your digestion with new food all the time. Eating too quickly results in food that is poorly chewed and a belly full of air, both of which cause bloating and indigestion. Chewing properly begins the digestive process right away and makes food more digestible. Eating when stressed, worried or angry triggers a stress response, i.e. the body’s fight-or-flight mode, which is terrible for digestion. The fight-or-flight mode is the opposite from the rest-and-digest mode. To harness the digestion-promoting rest-and-digest mode, make sure to eat when you feel calm, find a calm environment, and sit down.
Some clients of mine have found that this is all they need to keep their symptoms at bay! So, while they seem simple, these points are truly foundational and have an enormous effect on how well you digest and absorb your food.
What else for IBS?
Once the foundation is well in place, it’s important to find out if your diet is in balance, especially thinking of your individual symptoms. Balance means getting all the nutrients your body needs to be well while including food items that support easing your symptoms, and it also means that your microbiota gets all the food they need. Your gut microbes keep you well if you nourish them properly. Well-fed beneficial bacteria then send positive signals to the brain through the gut-brain axis, with health promoting effects.

A balanced diet is an optimal mix of protein, fat, and carbohydrates (including fiber), as well as vitamins, minerals and antioxidants. A plate method is a nice way of visualizing a balanced diet (see image above), but this also is a generalization that is not appropriate for everyone. It also doesn’t address fat in the diet.
What’s more, sometimes it’s not your diet that is the problem – there are situations when it doesn’t matter what you eat and your symptoms are difficult anyway. This is because IBS is caused by a problem in the way in which your gut and your brain talk to each other, and food is not exactly what causes this disruption. I talk about the gut-brain axis in a blogpost here, a great read!
Are your eating habits helping you ease IBS symptoms? Is your diet in balance?
If you are not sure, get in touch with me. During a 30-minute free gut health review I will give you the tools to build a diet that will keep your gut, and the rest of your body happy, but not only that. We’ll address your gut-brain axis also, for best results. Book your free call here.

Love,
Anna-Kaisa
PS. Don’t wait to get individualized advice for FREE! Book your call now.
PPS. Did you download my free Ebook “5 Easy Ways to Beat the Bloat” yet? These five ways are simple, yet effective in easing bloating that you can put to use right away.
I was at a networking lunch where the lady next to me, after hearing that I specialize in IBS and gut health, started talking to me about her experience on using Ozempic. You’ve heard of Ozempic, right? With the help of this drug, she lost 25 kg (55 lbs) in a year, but as a “side effect” her long term digestive issues were greatly improved.
Fascinating! I had heard about this in passing before, so I wanted to take a deeper look into the drug and whether this is a proven effect.
But first, what is Ozempic?
Ozempic is a brand name for the drug semaglutide, a prescription medication to help people with type 2 diabetes to better control their blood sugar levels, and more recently to help people lose weight. Blood sugar becomes lowered through the hormone insulin, which is released into the blood stream in larger amounts, and weight loss is becomes possible through lowered appetite. It’s also likely that eating sugary and fatty foods (and drinking alcohol) becomes less rewarding, leading to weight loss. (2)
Ozempic is a once weekly injection, and it acts as a GLP-1 agonist. This means that the drug mimics the action of the gut hormone GLP-1 (1). And here’s what explains the gut side effects: as a gut hormone it also helps regulate digestion – it decreases stomach movements and secretions, and slows down digestion.
Interestingly, L-cells that secrete GLP-1 in the gut have different functions depending on their location. In the small intestine, GLP-1 is released in response to nutrients (food) in the GI tract, but further down in the large intestine these cells become stimulated by bile acids, fiber, short chain fatty acids and gut microbes. In the same way, GLP-1 seems to slow things down higher in the intestines and speed things up lower down (5), although some studies suggest that also the large intestine becomes slower. GLP-1 has also been found to improve increased permeability in the large intestine, though the study was done in rats (6).

Ozempic digestive side effects
While the lady I talked to mentioned improvements in her gut issues, interestingly the most common side effects are digestive problems: nausea, constipation, diarrhea, abdominal pain and heartburn. (1) Furthermore, even more severe gut problems can be caused by Ozempic and the like - the risk of pancreatitis, stomach paralysis, bile issues and gut obstruction are increased. It’s not clear why this happens, but it probably has something to do with the ability of GLP-1 agonists to slow down the movements of the digestive tract. (3,6)
When it comes to IBS specifically, some evidence shows that GLP-1 levels are lower in people with constipation predominant IBS and these lower levels are connected also with abdominal pain. However, in a study with mice with something like IBS-C, GLP-1 levels where higher than in normal mice. (4)
Importantly, GLP-1 can worsen stress-related changes in intestinal motility and stimulate the HPA-axis (of which the end products are stress hormones). This is bad news, as stress is recognized as a major trigger of IBS. At the same time, GLP-1 may reduce abdominal pain. (4)

What does this all mean?
This all sounds a bit confusing, so what should you think about this all?
GLP-1 is certainly an important gut hormone that all of us have naturally, but medications that mimic this hormone to boost its function are not unproblematic. And while GLP-1 agonists act on the gastrointestinal tract, scientists are only beginning to explore whether they could be utilized as an IBS therapy at some point in the future. If you are someone who is considering, or already on Ozempic or something like it, please keep the severe gut side effects in mind, so that if your gut function changes drastically, or new symptoms arise, you get them checked out immediately.
Since supportive diet and lifestyle changes are necessary (and based on what the lady told me, often forgotten) even when on this medication, this is a factor to consider and maximize first. If you are not sure what this means, you can write to me.
Also, you can begin supporting your GLP-1 levels naturally by choosing foods that stimulate GLP-1 secretion, like eggs, avocado, olive oil, nuts, and high fiber foods (whole grains, vegetables) (7-12). There’s also some evidence that certain probiotics can enhance GLP-1 secretion, for example Akkermansia municiphila (12).

Get your doc to give you the full story
Many medications have side effects that affect the digestive system. Whether GLP-1 agonists are helpful or harmful depends on the individual. Importantly, talk with your doctor about the GI side effects to make sure the drug is suitable for you. If you are feeling confused, or unsure, ask follow up questions. In fact, any time you are at the doctor’s office and have questions, voice them out! Too often I hear people being disappointed with their doctors leaving them confused about what they should do, especially when it comes to IBS, so demand more detailed explanations. This is your health that we are talking about at the end of the day and it’s the doctors job to explain to you properly.
Thank you so much for reading about this timely topic! Be in touch if you have questions, or if you’d like a topic to be discussed here ([email protected]).

Love,
Anna-Kaisa
PS. Did you download my free ebook yet? Get it here.
PPS. Learn to Meditate –course 2.0 is starting in 3 weeks! If you want a method that gets better at mending your gut-brain axis with time (the root cause of IBS), this course is excellent for you. Sign up here - only $105!
References:
- Puckey, M. Ozempic. Drugs.com. 2025. https://www.drugs.com/ozempic.html accessed 3/6/2025
- Smith NK, Hackett TA, Galli A, Flynn CR. GLP-1: Molecular mechanisms and outcomes of a complex signaling system. Neurochem Int. 2019 Sep;128:94-105. doi: 10.1016/j.neuint.2019.04.010. Epub 2019 Apr 17. PMID: 31002893; PMCID: PMC7081944.
- Dewan, P. Weight Loss Drugs Ozempic and Wegovy Linked to Severe Gut Problems: Study Newsweek. https://www.newsweek.com/weight-loss-drugs-ozempic-wegovy-gut-problems-health-1832375 accessed 3/19/2025
- O'Malley D. Endocrine regulation of gut function - a role for glucagon-like peptide-1 in the pathophysiology of irritable bowel syndrome. Exp Physiol. 2019 Jan;104(1):3-10. doi: 10.1113/EP087443. Epub 2018 Dec 10. PMID: 30444291.
- Funayama T, Nozu T, Ishioh M, Igarashi S, Sumi C, Saito T, Toki Y, Hatayama M, Yamamoto M, Shindo M, Tanabe H, Okumura T. Centrally administered GLP-1 analogue improves intestinal barrier function through the brain orexin and the vagal pathway in rats. Brain Res. 2023 Jun 15;1809:148371. doi: 10.1016/j.brainres.2023.148371. Epub 2023 Apr 17. PMID: 37076092.
- Holst, J. J., Andersen, D. B., & Grunddal, K. V. (2021). Actions of glucagon‐like peptide‐1 receptor ligands in the gut. British Journal of Pharmacology, 179(4), 727-742. https://doi.org/10.1111/bph.15611
- Santos-Hernández M, Amigo L, Recio I. Induction of CCK and GLP-1 release in enteroendocrine cells by egg white peptides generated during gastrointestinal digestion. Food Chem. 2020 May 30;329:127188. doi: 10.1016/j.foodchem.2020.127188. Epub ahead of print. PMID: 32516710.
- Bodnaruc AM, Prud'homme D, Blanchet R, Giroux I. Nutritional modulation of endogenous glucagon-like peptide-1 secretion: a review. Nutr Metab (Lond). 2016 Dec 9;13:92. doi: 10.1186/s12986-016-0153-3. PMID: 27990172; PMCID: PMC5148911.
- Zhu L, Huang Y, Edirisinghe I, Park E, Burton-Freeman B. Using the Avocado to Test the Satiety Effects of a Fat-Fiber Combination in Place of Carbohydrate Energy in a Breakfast Meal in Overweight and Obese Men and Women: A Randomized Clinical Trial. Nutrients. 2019 Apr 26;11(5):952. doi: 10.3390/nu11050952. PMID: 31035472; PMCID: PMC6567160.
- Hira T, Trakooncharoenvit A, Taguchi H, Hara H. Improvement of Glucose Tolerance by Food Factors Having Glucagon-Like Peptide-1 Releasing Activity. Int J Mol Sci. 2021 Jun 21;22(12):6623. doi: 10.3390/ijms22126623. PMID: 34205659; PMCID: PMC8235588.
- Indarto D, Rochmah DN, Wiboworini B, Pratama YM, Wibowo YC. Effects of Vegetables Consumption Before Carbohydrates on Blood Glucose and GLP-1 Levels Among Diabetic Patients in Indonesia. Int J Prev Med. 2022 Nov 23;13:144. doi: 10.4103/ijpvm.IJPVM_704_20. PMID: 36618536; PMCID: PMC9811965.
- Cani PD, Knauf C. A newly identified protein from Akkermansia muciniphila stimulates GLP-1 secretion. Cell Metab. 2021 Jun 1;33(6):1073-1075. doi: 10.1016/j.cmet.2021.05.004. PMID: 34077715.
The low FODMAP diet has been a first line treatment for IBS for some time now. It makes sense, as there are studies showing that about 2/3 of people with IBS get at least some relief from symptoms (constipation, diarrhea, bloating, abdominal pain) while on the diet.
But here’s the truth: food doesn’t really actually cause IBS! And while the diet shows improvements in IBS symptoms, it’s not a diet that everyone with IBS should even try. It seems that medical providers are not always considering the pros and cons of the diet fully when recommending the diet to patients, nor do they understand the full impact of the different aspects of your diet on IBS symptoms, not just what the foods you eat are. When tests come out clear you (usually) get an IBS diagnosis and then the doctor just hands you a piece of paper that goes through the FODMAP diet and expects you to be able to execute the diet without issue.

For one, this is not really the way to fully learn the diet to begin with. It is too complicated to understand from just a handout.
And for two, not everyone should try the low FODMAP diet. Here is why:
- FODMAPs don't cause IBS. FODMAPs are small fibers that your digestion can't break down, and so they travel into your large intestine intact and are then digested by your gut microbes instead. This causes gas formation. The thing is that this doesn’t just happen in people with IBS. It happens in everyone, but the difference is that people with IBS have visceral hypersensitivity, which means that they are more sensitive to everything that is going on in the gut, including gas. What you need to work on is to reduce sensitivity, not just to remove anything and everything that could be more difficult to digest. When sensitivity improves, your tolerance to food improves as well. How do you reduce sensitivity? You need to address the root cause of IBS.
- The low FODMAP diet is a complicated diet that causes stress. We know that stress is detrimental to digestion and gut health, and so anything that increases stress is counterproductive to managing IBS symptoms. This is also the reason why working with a dietitian is important if you do decide to try the diet. You don't want to waste time and effort doing the diet wrong and stressing out about it.
- Big diet restrictions, such as the low FODMAP diet, can cause fear toward food. Fear is something that triggers a stress response in the body, and as I mentioned above, stress is really not helpful to your symptoms. If you feel fear toward eating and food, this is your sign to chat with an expert.
- Removing many foods from your diet increases your risk of nutrient deficiencies. This is another reason why you should always work with a dietitian - they will make sure that you will find foods that will ensure a balanced diet, even with big diet restrictions.
- When restricting your diet because of gut symptoms, what happens often is that you become more observant of your gut, which makes you more sensitive. Increased sensitivity is again counterproductive to what you're actually trying to do, which is to manage your IBS symptoms better.
- Very importantly, the low FODMAP diet can change your gut microbiota in undesired ways. There are studies that show that especially Bifidobacteria decrease with the low FODMAP diet and this is again counterproductive to what you are trying to do. Microbiota plays a big role in the gut-brain axis. Negative changes in the gut microbiota negatively impact IBS and the gut-brain axis also.
I don't mean that the low FODMAP diet is never a good idea or that no one should try it. What I am saying is that we should be a lot more careful when we consider the possibility, as it is far from a risk free diet. It might even make your symptoms worse! And you should always remember that these kinds of diet changes are only bandaids, they don’t fix the root cause of your symptoms.

If you decide to do it, you always need the help of a dietitian to do it right so that you can stress less and waste less time and effort. Not to mention get actual reliable information from the diet. If you are not doing it right, or if it’s not the right step for you to take (now or ever), you can’t get results from the diet that truly guide you toward food choices that at least won’t make your symptoms worse.
Also, IBS is now classified as a disorder of gut-brain interaction. While food certainly affect this interaction, it is probably not in the ways that you think it does. What is more important than jumping into the low FODMAP diet is to look at everything else that is going on in your life also. Such as sleep, exercise, rest, stress levels, etc. All these things can have quite the big impact on your digestion, especially sleep and stress.

So, my recommendation is that before you try the low FODMAP diet, check that your diet is balanced in other ways and think about your stress levels and how you are sleeping. When you get those 3 in order, the chances are good that you will feel better without needing to follow a difficult and highly restrictive diet.
Because IBS is such a complicated digestive disorder, it is very useful to chat about these things with an expert instead of trying to manage them on your own. You can save a lot of time and effort when you have a clear road map to follow. Call me for free to find out what that road map might look like for you, just go here to book your free strategy session.
Thank you so much for reading! I hope this was helpful to you. Please be in touch if there's anything else I can do for you.
Whatever you decide to do, don't lose hope - I believe that there's always something that will help you improve your symptoms. Even if it might take some trial and error to find.
Love,
Anna-Kaisa
PS. I have many resources that you can download for free. Did you get them yet? Here’s the “Secret Solution for IBS” ebook for example - it’s filled with useful information to help you better manage your IBS symptoms without the low FODMAP diet.
PPS. Take advantage of your free call! Let’s strategize together and build you a roadmap toward IBS freedom.

In my extensive research on IBS, I’ve come across all kinds of information and claims on the topic. The cause of IBS seems especially debated, some doctors agreeing with me in that stress can cause IBS, while others believing stress has nothing to do with it.
The title of this post is an argument made by a doctor against the idea that stress causes IBS. He felt that stress makes everything worse, so if you have IBS, the symptoms just get worse when you are stressed out, just like how all your health issues would.
I agree that stress makes everything worse. But I do believe stress can also cause IBS.
In short:
- There is much evidence to show that a large proportion of people with IBS have trauma in their past (extreme stress)
- The IBS diagnosis was made right after a period of severe stress in many, if not most, cases. I’ve seen this with my clients time and again.
- Stress can lead to all the classic IBS symptoms. This is a fact.
Furthermore, scientists agree that stress can cause a whole host of symptoms, NOT ONLY digestive problems and all the classic IBS symptoms of bloating, diarrhea, constipation and abdominal pain, but also headaches, muscle tension, hives, high blood pressure, dizziness….
Everyone has stress (at least sometimes), then why doesn’t everyone have IBS?
It’s a matter of stress manifesting in different ways in different people. I don’t know why someone gets migraines from stress and someone else horrendous bloating, it’s probably a sum of many things that are different between individuals.
It seems most of us have experienced gut symptoms from stressful episodes, especially when feeling nervous from having to perform in front of people, be it a speech or a sports competition. Me included! The symptoms just don’t reach the severity or frequency to qualify for an official IBS diagnosis every time.
"Everyone has IBS"
I recently chatted with a gastropsychologist (a psychologist specializing in IBS and other digestive disorders), and it was her thought that “everyone has IBS”. It's an interesting way to think of it, and essentially it speaks to the stress reaction being a universal mechanism. Then, if stress is severe enough and passes a certain individual threshold, everyone will get GI symptoms of some kind!
So, don’t believe when someone even of authority says that stress doesn’t cause IBS. Sure, there are many things at play, and stress might not be the only ingredient needed to “make” IBS, but to say it has no role at all in IBS to me is impossible.
If you are serious about taking charge of your IBS, talk to me. I offer free 30-minute consultations (no strings attached!) to give you a chance to talk to an expert about your situation. You’ll gain valuable advice on your next steps toward IBS freedom, and a chance to have expert guidance going forward, if you so choose.
How are your stress levels these days? It’s hard to remain centered in this tumultuous world!
Love,
Anna-Kaisa
PS. Did you download my free “5 Easy Ways to Beat the Bloat” -ebook yet? Go here to get it!

Could the answer to IBS lie in the ancient practice of meditation?
IBS is a world-wide problem and the most common gastrointestinal disorder.
For a long time, irritable bowel syndrome has just been thought of as a functional problem: there’s nothing measurably, or visibly wrong with the intestines, so labeling IBS as a functional problem is almost like a shrug from the experts.
Now, IBS has earned a new classification: a disorder of gut-brain interaction. So, instead of IBS being a functional problem, there’s actually something physical that becomes disrupted – it’s just not visible to the naked eye.
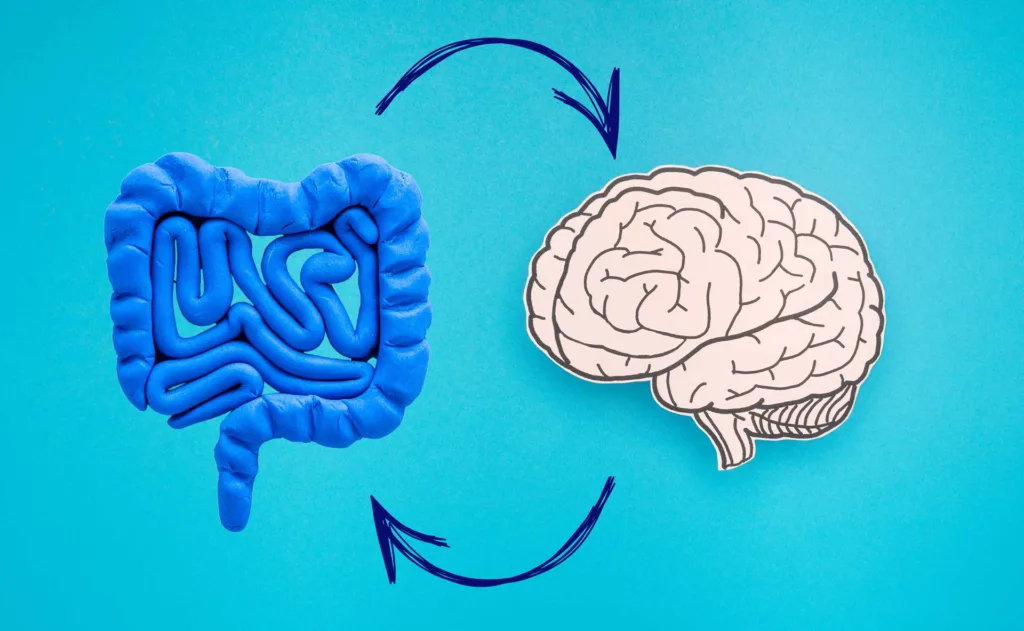
What is gut-brain interaction? It is the two-way communication highway between your brain and your gut. It’s also called “gut-brain axis”. When the connection is disrupted, there are misunderstandings and overreactions that lead to IBS symptoms. You can read more about the gut-brain axis in this blog post.
What disrupts the gut-brain interaction? Many things, but a big culprit looks to be stress (1). Stress causes stress hormones to surge in the body, which turn digestion off. With a lower digestive “fire”, food digests poorly, leading to abdominal pain, diarrhea/constipation and/or bloating.
To make matters worse, the brains of people with IBS are wired in ways that make them more sensitive to stress, triggering a stress response more easily, which causes a difficult situation to turn into gut symptoms more easily as well. (2)
Solution? To mend the gut-brain interaction through stress release practices and mindset shifts.
My favorite method is meditation. It feels like an antidote to pretty much anything, sort of how exercise and good nutrition are.
When it comes to IBS, there are studies linking meditation to improved IBS symptoms, like improved abdominal pain and improved quality of life. (3)

And what I’m really excited about, is meditation’s ability to change the brain to withstand stress better (4). This means that while stress is not going to go away, you cope better with stress, and a stressful situation less easily leads to IBS symptoms. Naturally, these effects come from a long-term practice. But, even a one-time practice of a few minutes of meditation can measurably reduce stress. (5)
Personally, after 15 years of practice, daily meditation has become my secret weapon. Not only do I feel great while meditating (though not always, sometimes my brain is just too restless), I’ve noticed in general feeling calmer, more empathetic, and having a better emotional control than I used to. It feels like my brain gets triggered less easily.
One of the meditation techniques I particularly love is Hong Sau (Sau pronounced “saw”). It’s a technique of attentive focus on the breath. Since the breath is always there, it becomes an excellent object for meditation (no, meditation is not about blanking the mind). A focused mind is a calm mind, and a calm breath leads to a calm mind and vice versa. Or how do you breathe when you are reading a book with deep focus?
I’m teaching the Hong Sau meditation technique live online starting today on Wednesday January 8th 2025. There’s still time to sign up! Even if you miss the first class, you can still participate live in the remaining four. All the sessions will be recorded, so you’ll get the recording of the first session, and they will be made available for purchase as a full course after the live course is finished. Go here for more info. Sign up by emailing me at [email protected]
Questions? You got my email address.
Let’s make the year 2025 the best one yet! Let’s start by taking up meditation, or some other stress release practice, and cultivating the belief that improvement is possible – I really do believe that. Even if you feel like you’ve tried everything, something will help you, if you keep working at it.

Love,
Anna-Kaisa
References
- Cryan JF, O'Riordan KJ, Cowan CSM, Sandhu KV, Bastiaanssen TFS, Boehme M, Codagnone MG, Cussotto S, Fulling C, Golubeva AV, Guzzetta KE, Jaggar M, Long-Smith CM, Lyte JM, Martin JA, Molinero-Perez A, Moloney G, Morelli E, Morillas E, O'Connor R, Cruz-Pereira JS, Peterson VL, Rea K, Ritz NL, Sherwin E, Spichak S, Teichman EM, van de Wouw M, Ventura-Silva AP, Wallace-Fitzsimons SE, Hyland N, Clarke G, Dinan TG. The Microbiota-Gut-Brain Axis. Physiol Rev. 2019 Oct 1;99(4):1877-2013. doi: 10.1152/physrev.00018.2018. PMID: 31460832.
- Mayer EA, Ryu HJ, Bhatt RR. The neurobiology of irritable bowel syndrome. Mol Psychiatry. 2023 Apr;28(4):1451-1465. doi: 10.1038/s41380-023-01972-w. Epub 2023 Feb 2. PMID: 36732586; PMCID: PMC10208985.
- Baboș CI, Leucuța DC, Dumitrașcu DL. Meditation and Irritable Bowel Syndrome, a Systematic Review and Meta-Analysis. J Clin Med. 2022 Nov 2;11(21):6516. doi: 10.3390/jcm11216516. PMID: 36362745; PMCID: PMC9658118.
- Taren AA, Gianaros PJ, Greco CM, Lindsay EK, Fairgrieve A, Brown KW, Rosen RK, Ferris JL, Julson E, Marsland AL, Bursley JK, Ramsburg J, Creswell JD. Mindfulness meditation training alters stress-related amygdala resting state functional connectivity: a randomized controlled trial. Soc Cogn Affect Neurosci. 2015 Dec;10(12):1758-68. doi: 10.1093/scan/nsv066. Epub 2015 Jun 5. PMID: 26048176; PMCID: PMC4666115.
- Mandlik GV, Siopis G, Nguyen B, Ding D, Edwards KM. Effect of a single session of yoga and meditation on stress reactivity: A systematic review. Stress Health. 2024 Jun;40(3):e3324. doi: 10.1002/smi.3324. Epub 2023 Oct 11. PMID: 37822096.
I’ve recently noticed a diet that is trending – the carnivore diet – not just among people in general, but also among people with IBS. Being a dietitian makes me very interested in all diets, but I must say this takes the cake. This diet seems to be completely counterintuitive, as it goes against all dietary guidelines out there, so why do people try it anyway?
It's because some people who follow the carnivore diet report feeling much better after switching. They feel more energetic and lighter than before. They report that their IBS symptoms get better, even disappear in some cases. As a registered dietitian, this is hard hard for me to believe, so let’s dig in and see what is going on here.

The Carnivore Diet: A Closer Look
Let’s first find out what this diet is. This diet is almost exactly as it sounds: it is all meat, fish and chicken. You are also allowed a little bit of cheese, heavy cream and eggs. Fat sources are lard and tallow, although some allow plant oils in the diet also. You can drink unsweetened coffee and tea and add spices that contain no carbs.
Basically, this diet is an extremely low carbohydrate diet, very high in protein, and high in fat. It is not possible to get all the nutrients your body needs from this diet, especially vitamin C, B vitamins, vitamin K and calcium, unless you include a variety of organ meats in your diet every day, like liver, kidney, and brain. For omega-3 fatty acids, it’s important to eat fatty fish, like salmon. Unless you drink coffee or tea, this diet contains hardly any antioxidants - these are highly beneficial for your health as they fight free radicals that damage your tissues. Animal foods contain no fiber that are needed to support the health of the gut microbiota.
To sum up, the carnivore diet is a highly restrictive eating plan that consists of 99% animal-based foods and carries with it a high risk of malnutrition. It’s not a diet that any dietitian or doctor can recommend to be followed. How is it possible then, to feel better with this diet?
Why you might feel better
There are no objective studies done, so I can’t say anything for sure, but I have a few theories why someone might feel better.
- You eat hardly any processed food and no sugar. Processed food is a big problem in today’s world. These foods usually contain additives, sugar, and hardly any vital nutrients, and so they are harmful to health. People who follow the carnivore diet are likely to eat a lot less processed food, perhaps even none, unless they choose deli meats and sausages etc. on their plate.
- Ketosis. The carnivore diet contains close to 0 grams of carbohydrate, which means the body must go into ketosis to survive. People on a ketogenic diet report feeling more alert (though not always!). Ketogenic diets also increase fat loss in the body, which helps lose weight and may help make you feel better (at least in the short term).
- Placebo effect. It is a big dietary change, and if you are expecting to feel better, the placebo effect can help you achieve this. At least for a while. Placebo effect tends to lose power long term.
- No carb fermentation. Gut symptoms may improve as there is no fiber for the gut microbes to process and make gas from – bloating and flatulence improve. However, a diet with no fiber, and without green/herbal tea no polyphenols either, cause negative changes to the composition of the gut microbiota (=dysbiosis). The lack of fiber tends to lead to constipation, and some people might even experience diarrhea caused by the dysbiosis.
It’s important to note, however, that there is no guarantee that you will continue feeling better in the long term. I’m almost certain the feeling will go away quickly, as the gut microbiota changes will affect your health negatively. Scientists can’t even study this diet properly, as it is unethical to conduct a study on a diet that is known to be risky. Here are some reasons why it is highly risky to follow the carnivore diet, especially for longer than a few days.

The risks involved
- Who knows what this does in the long term! There are no studies, and objective studies are not possible because of ethical reasons as mentioned above. Researchers would have to rely on a small group of volunteers, and so there would be many biases that come from a non-random study groups making results untrustworthy.
- In the long term, you will very likely get nutrition deficiencies without supplementation.
- No fiber in the diet leads to gut microbiota dysbiosis, which leads to health problems
- Gut microbes will need to process proteins and amino acids instead, leading to production of potentially harmful compounds.
- High meat consumption is linked to a host of health problems, like gout, osteoporosis, and kidney stones, and even colon cancer, whereas plant rich diets are linked to longevity and lower risk of chronic illnesses.
- No antioxidants at all, unless tea/coffee is added to the diet. Antioxidants fight free radicals and tissue damage.
- Humans are not actually carnivores, we are omnivores. Just compare the digestive systems of a wolf and a human. It’s not built to process only animal protein.
- Very high protein content. Excess protein will be turned into carbs and other molecules, and getting rid of protein waste products is very tough on the body. Kidneys will be taking a hit in the long term.
- The diet is not sustainable, you’ll get cravings eventually and it will be hard to maintain the diet. Resuming to your normal diet after being on a carnivore diet can cause you to regain all the weight you had lost, and sometimes gain even more.
- Following the diet increases the risk of disordered eating for people prone to them.
- Constipation from no fiber / diarrhea from changed microbiota.
Who absolutely should not try this diet

I wouldn’t recommend anyone following the carnivore diet, but people who are pregnant, lactating, have heart disease, kidney disease and potentially diabetes should not try this diet. Some experts also include people with IBS in this group, as the digestive system needs fiber to function normally.
But what about the Inuit?
The carnivore diet (or any meat-heavy diet for that matter) is against the dietary recommendations of any given country in the world. But then we have Inuits who mostly eat fish and meat. They seem to do well on this diet. So why shouldn’t others do the same?
This is an excellent question! Here’s what I found.
The reason for why the Inuit have been thriving on a diet that is high in animal protein is a result of thousands of years of genetic adaptation. These genes help the Inuit utilize high-fat diets well, and these genes are not commonly found in Europeans for example.

However, it’s important to note that the traditional Inuit diet is not a carnivore diet, it also includes local plant foods, studies are estimating 8-50% carbohydrate. Also, the Inuit eat lots of marine mammals and fish, including their internal organs, which helps provide more of the nutrients the body needs.
It has been thought that heart disease doesn’t exist among the Inuit population, but this might not be the case. Another problem with this diet is also that it doesn’t promote bone health - the Inuit have been found to have very poor bone health and early onset osteoporosis.
What to do instead
If you have IBS, and are seeking a diet that minimizes symptoms, it shouldn't be the carnivore diet. It might not be the low FODMAP diet either. What you need is a balanced, highly individualized diet that takes into account much more than just your gut symptoms, such as your age, gender, background history, habits, skills and so on. This is what dietitians do – they look at your diet from all angles and recommend changes to support your gut health, your overall health and your wellbeing.
If you are considering trying out an extreme diet like the carnivore diet, it is a sign to talk to an IBS dietitian and get real solutions that bring you real results, without risking your long term health. Book a free gut health review with me to kickstart your journey to finding your very own, best possible IBS diet.
With love,
Anna-Kaisa

PS. If you haven’t yet, download my free “5 Easy Ways to Beat the Bloat” guide packed with actionable tips that you can start applying in your day to day life right away.
PPS. Let’s chat! There is a right IBS diet for you out there. Book your free gut health review now!
References:
- LeWine, H. E., What is the carnivore diet? Harvard Health Publishing. 2024. Accessed 11/20/2024
- Eagle, R, medically reviewed by Seitz, A. Carnivore diet: What it is and how to do it. 2020. https://www.medicalnewstoday.com/articles/carnivore-diet accessed 11/20/2024
- Campbell, T. Masai and Inuit High-Protein Diets: A Closer Look. NutritionStudies.org. Accessed 11/20/2024
- Fumagalli M, Moltke I, Grarup N, Racimo F, Bjerregaard P, Jørgensen ME, Korneliussen TS, Gerbault P, Skotte L, Linneberg A, Christensen C, Brandslund I, Jørgensen T, Huerta-Sánchez E, Schmidt EB, Pedersen O, Hansen T, Albrechtsen A, Nielsen R. Greenlandic Inuit show genetic signatures of diet and climate adaptation. Science. 2015 Sep 18;349(6254):1343-7. doi: 10.1126/science.aab2319. PMID: 26383953.
- Oliphant K, Allen-Vercoe E. Macronutrient metabolism by the human gut microbiome: major fermentation by-products and their impact on host health. Microbiome. 2019 Jun 13;7(1):91. doi: 10.1186/s40168-019-0704-8. PMID: 31196177; PMCID: PMC6567490.
To truly manage IBS, you need to fix the way your brain and your gut talk to each other.
When talking about irritable bowel syndrome and IBS symptoms (abdominal pain, bloating, diarrhea, constipation), the discussion is not complete without considering the gut-brain axis. Especially since IBS experts are now calling the syndrome a disorder of gut-brain interaction. It’s a fascinating subject that reminds you how everything in the body affects everything - in good and in bad. This applies also to managing IBS symptoms: it’s not enough to focus on one aspect of gut health, like your diet, but also sleep, circadian rhythms, exercise, stress, and even thoughts have to be assessed as all of these affect the gut-brain axis.
What is the gut-brain axis
Often called the gut-brain-microbiota axis, the gut-brain axis is the communication channel between the gut and the brain, the two-directional phone line between the two.
Your gut and your brain are talking to each other all the time! The main office (the brain) wants to know what the branch office is doing (the gut) and give orders if need be. They relay information back and forth about gut processes, hunger, satiety, stress, and feelings, just to name a few.
Problems in this information exchange are linked to irritable bowel syndrome and other “functional” gut problems, immune function, sleep problems, mood disorders, neurodegenerative diseases, and even obesity.
How are your gut and your brain connected?
It’s not simple. Many processes are involved:
- Central nervous system (brain and spinal cord): both the sympathetic (stress response) and the parasympathetic (rest response) branches of the autonomic nervous system are involved, especially the vagus nerve
- Enteric nervous system (gut’s own nervous system)
- Endocrine pathways (hormones): such as HPA-axis with cortisol (stress hormone), gut hormones like ghrelin (hunger hormone) and leptin (regulates appetite)
- Immune system of the gut: cytokines (inflammation controlling molecules)
- Microbiota (gut microbes) and the molecules they produce, like short chain fatty acids and neurotransmitters

To simplify, what you need to know is that
- The enteric nervous system takes care of digestion, but the brain can override its functioning in stressful situations.
- The vagus nerve is the main information pathway between the brain and the gut, and there is evidence to show that it’s not working well in people with IBS.
- Gut microbes are highly important, and how you take care of them makes an impact on the gut-brain axis level also.
What disrupts the gut-brain axis
It’s not completely clear how this happens, but it seems stress plays a big role, as does the health of the gut microbiota. Your gut microbes are affected by your lifestyle and your diet, both in helpful and harmful ways. It is thought that dysbiosis of the gut microbiota (negative changes in your gut microbes) can cause problems in the gut-brain axis, but it is not clear whether dysbiosis happens first, or whether the disruption of the gut-brain axis causes the dysbiosis.
IBS can become triggered by a gut infection, which could support the idea that your gut microbe balance becomes disrupted first, but an infection also causes inflammation which the immune system controls. Gut infection is also a source of stress, and a sensitive brain may overreact to infection signals coming from the gut, starting a feedback loop that causes IBS. So, it’s not clear.
The brain then is responsible for assessing whether we are in danger or not, but your lifestyle and your diet can also affect your stress sensitivity, or how readily a stress response is triggered in the body. A typical Western diet and an irregular lifestyle with sleep deprivation could make you more sensitive to stress.
Stress sensitivity
People who have had lots of stress in their lives, whether in childhood or in adulthood, become more sensitive to stress, and are at a higher risk for developing IBS. Studies show that over time their brains have adapted to stress in an unhelpful way, which explains this increased sensitivity, and probably also why not everyone with stress has IBS.
Additionally, people with IBS tend to have these similar structural brain changes and increased stress sensitivity also, and a history of highly stressful life periods. For example, I had a client whose gut symptoms began after a serious natural disaster hit her country. This all suggests that chronic stress wreaks havoc on the gut-brain axis and promotes chronic gut issues, like IBS.
What’s more, it’s relatively common that anxiety and depression happen together with IBS, both probably feeding the other. What came first, however, is not clear.
Looking after the gut-brain axis
Everyone can benefit from taking good care of the gut-brain axis, but this is especially important for people with IBS and other functional digestive disorders. It seems that gut symptoms are like the tip of an iceberg – your gut-brain axis may have been disrupted for a while before gut symptoms surface!
How to nurture your gut-brain axis:
- Feed your good gut bacteria with a balanced diet rich in fiber
- Support digestive processes by eating regularly, avoiding overeating, drinking enough fluids, limiting alcohol consumption
- Stimulate vagus nerve and calm the nervous system with stress releasing activities
- Activate brain areas that lower stress sensitivity: breathing exercises, meditation
- Work on your mindset to reduce catastrophizing, expecting problems etc.
- Pay less attention to your gut symptoms
- Nurture body’s processes: keep regular daily rhythms with sleep, meal patterns and exercise, do your best to sleep well
- Perhaps specific supplements, like probiotics can help
It’s a lot! But not impossible to do.

Strong gut-brain axis plan
The first step is to map out honestly how you are doing in these different areas listed above.
The second step is to make a plan: what needs to change and in what order. Consider what might be easier to start with, or what might make the biggest impact.
But you don’t have to figure this out on your own. Nurturing a sturdy gut-brain axis and relieving IBS symptoms in the process is what I do. If you are not sure, let’s chat. You will have the opportunity to tell an expert about your situation, and I will go over your best next steps without you having to commit to a program. I want to make sure you and I are a good match before you invest anything in working together. Book you free consultation here.
I hope you enjoyed learning about the all-important gut-brain axis! If you are feeling overwhelmed by this, just remember that even small adjustments to diet, lifestyle, thought patterns and stress sensitivity can make a big difference. Check out all of my free resources (scroll down my home page) - they provide lots of tips to get going with.
Thank you for reading!
Love,
Anna-Kaisa

PS: Book your free 30-minute consultation here!
PPS: Feeling bloated? Get your copy of the free “5 Easy Ways to Beat the Bloat” guide here!
References
- Chen M, Ruan G, Chen L, Ying S, Li G, Xu F, Xiao Z, Tian Y, Lv L, Ping Y, Cheng Y, Wei Y. Neurotransmitter and Intestinal Interactions: Focus on the Microbiota-Gut-Brain Axis in Irritable Bowel Syndrome. Front Endocrinol (Lausanne). 2022 Feb 16;13:817100. doi: 10.3389/fendo.2022.817100. PMID: 35250873; PMCID: PMC8888441.
- Mayer EA, Nance K, Chen S. The Gut-Brain Axis. Annu Rev Med. 2022 Jan 27;73:439-453. doi: 10.1146/annurev-med-042320-014032. Epub 2021 Oct 20. PMID: 34669431.
- Mayer EA, Labus JS, Tillisch K, Cole SW, Baldi P. Towards a systems view of IBS. Nat Rev Gastroenterol Hepatol. 2015 Oct;12(10):592-605. doi: 10.1038/nrgastro.2015.121. Epub 2015 Aug 25. PMID: 26303675; PMCID: PMC5001844.
- Karakan T, Ozkul C, Küpeli Akkol E, Bilici S, Sobarzo-Sánchez E, Capasso R. Gut-Brain-Microbiota Axis: Antibiotics and Functional Gastrointestinal Disorders. Nutrients. 2021 Jan 27;13(2):389. doi: 10.3390/nu13020389. PMID: 33513791; PMCID: PMC7910879.
- Sun LJ, Li JN, Nie YZ. Gut hormones in microbiota-gut-brain cross-talk. Chin Med J (Engl). 2020 Apr 5;133(7):826-833. doi: 10.1097/CM9.0000000000000706. PMID: 32132364; PMCID: PMC7147657.
If you are wondering the answer to this question, you are not alone. There are millions of people out there experiencing gut symptoms and wondering if they should be worried about them.
The most common IBS symptoms are:
- Abdominal pain
- Bloating and/or distention of the belly
- Constipation
- Diarrhea
The way IBS is diagnosed, in order for your symptoms to “qualify” as IBS, abdominal pain must be present. It can be crampy, aching, and even quite severe. Often it is triggered or made worse by food, bowel movements and stress.

This abdominal pain is also often associated with a change in stool frequency or consistency. It typically gets better after having a bowel movement, and it would actually be concerning if it didn’t. Since abdominal pain in IBS is considered visceral pain, you’ll often feel pain in the midline of the body.
Bloating is a feeling of tightness and fullness of the abdomen, and your belly feels like it is visibly bigger, even though it may or may not be so. Distention is the term for your belly protruding more than usual with measurable increase in the abdominal circumference. People feel like they have a balloon in their belly, or that they are pregnant when they are not pregnant. Bloating and distention can cause discomfort and it may feel embarrassing.
Constipation is an infrequent bowel movement pattern, in which you have a bowel movement less than three times a week. Though it seems to me you can feel constipated even if you move your bowels daily. Constipation usually goes hand in hand with small, hard, pebble-like stools and they are hard to pass. You might feel like your bowels are not emptying fully.
Diarrhea is the opposite of constipation. It refers to loose, watery stools, more than three times per day. Diarrhea could also cause urgency - you can’t wait a minute longer to go to the bathroom or else an accident might happen.

These symptoms can be very debilitating. They might also change from day to day, one day having constipation and the next diarrhea. People experiencing IBS symptoms may feel like they need to watch closely what they eat, not stray too far from the toilet, and avoid going out to see friends, travel or eat out.
If you’ve been experiencing IBS symptoms for longer than a few weeks, or less if the symptoms are very difficult, I encourage you to go get them checked out. Then, even if your symptoms didn’t fulfill the IBS diagnostic criteria, you’d find out whether there’s something more serious going on, or whether there’s nothing to worry about. Either way, it’s better to be in the know than to be guessing!
If you have been diagnosed with IBS, but are not sure whether this is the right diagnosis, I would again encourage you to speak with your doctor. Ask how they diagnosed the disorder and voice your concerns. The end result (should be) that your doctor will either order more tests, or explain to you more thoroughly their thinking process, so that you can rest assured the right call has been made and that you can begin to apply the right therapies.
If you end up being diagnosed with IBS, or even if you’re not, I have what you need to improve your symptoms. Sign up to my IBSwise program, or if you’d like a more individualized approach, book a free 30-minute chat to discuss your next move.
Whatever you do, don’t be left alone with your symptoms! There is so much you can do to ease them.
Love,
Anna-Kaisa

I had the pleasure of being hosted in an educational webinar to my fellow dietitians in Finland this past week. The topic was the connection between stress and irritable bowel syndrome. I had the opportunity to speak to over 50 of my peers about this subject that important and yet, significantly overlooked.
Many studies show the intimate connection between stress and our digestive system through the gut-brain axis. Many factors affect digestion, including the food we eat, but when stress levels are high, what we eat makes no difference – we will have gut trouble until we address the stress. Eating or not eating results in pain, bloating and either diarrhea or constipation. So yes, I can tell you that stress causes gut problems, likely also IBS, and it can certainly make it worse!
In this presentation that I gave to my fellow dietitians, I talked about the science behind stress and IBS. I went over the mechanisms through which stress affects the gut. For example, stress can cause inflammation in the gut, disrupt your gut microbiota and make the gut more sensitive to what’s happening within it, even to normal things, like a small amount of gas from bacterial fermentation of whole grains (which is good for us!).
I also went over different kinds of stress release techniques and the scientific evidence that exists for these different methods. Many different techniques are found to improve IBS symptoms, which leads me to believe that every one of us, with or without IBS, should have a stress release routine to follow every single day.
And this is not just for gut health. I believe it is impossible to have good health without stress management. It also doesn't have to be difficult, complex, or time-consuming. It can simply mean taking deep breaths before each meal, or questioning negative thoughts. Or it could be about practicing yoga and meditation regularly. Even taking a walk, taking care of your diet, sleeping well, drinking enough fluid, and spending time outdoors can do wonders to stress.
All my clients have experienced significant improvements in their gut issues when they have not only paid attention to their diet, but also started a daily stress release routine. For example, taking time to eat in peace instead of hurrying through each meal has made a big difference! Breathing exercises have also been a very central part of their stress release routines and my clients say they have been “life saving”.
If you are thinking “I don't have any stress”, I would suggest to question this, because everyone has some stress, and stress is not always felt on a mental level. Physical symptoms can be the only telltale signs of stress in your life. So, even if you don't feel like you're stressed out but are suffering from a lot of ailments, including gut issues, try stress release anyway because more than likely it will help you.
Furthermore, it will not only help your gut health, but your well-being overall.

Everything affects everything, so only adjusting your diet is not enough for true health. We need to look at every aspect of life to truly find the causes for our symptoms and the best solutions.
You can start by signing up to IBSwise and exploring the different stress release techniques I offer there, or visit my Instagram page to try the box breathing exercise that I have pinned to the top of the posts.
Any questions? Just comment below, or email me at [email protected].
Thank you for reading!
Love,
Anna-Kaisa

PS: I host free 15-minute stress release sessions on Thursdays, every other week. The next session is September 5. You can register here for the next session, and email me if you’d like a link to watch the recording from the last session.
PPS: I have lots of free stuff you can download! For example, you can get the free guide “5 Easy Ways to Beat the Bloat” here!
Earlier this month National Geographic published an article headlined “Why women are more likely to have IBS”. I love that big publications such as National Geographic are paying attention to irritable bowel syndrome, as it is so common, and as there is so much misleading information out there. Big publications could help bust some of that misinformation.

The article aimed to explore why more women than men have IBS, and to discuss some of the treatment options. Since the comments below the original Instagram post, where I first spotted the article, seemed to point out some discrepancies, I thought I’d chime in and expand on some of the unclear points. Here are some of my thoughts:
- According to Dr. Raj, a gastroenterologist, IBS is a diagnosis of exclusion – more severe illnesses with overlapping symptoms need to be ruled out before an IBS diagnosis can be made. My experience: not all doctors test for everything, like cancer and IBD. This is probably to save resources, especially in a public healthcare setting, where money is tight. However, this leads to patients feeling unsure of their diagnosis. It's one of the reasons why it's so important to be able to advocate for yourself when talking to doctors. When you know a bit about what to expect, you will feel more empowered to ask the right questions and get the help you need (one of the reasons I created IBSwise). Here’s my wish to doctors seeing patients with IBS and these kinds of gut issues: spend time explaining your decisions on testing and recommendations so that people feel heard, and can understand and accept their diagnosis and thus go for correct treatments, instead of wasting time and money looking in the wrong places.
- The reason why women are more likely to have IBS is hormones. This I can agree with. I wrote a blogpost about it.
- Another reason for women being more susceptible to IBS: sensitivity to stress. Yes, seems true. I was also glad to see stress mentioned early in the article, as this is also what I have found in my IBS research. Stress is a real culprit in IBS, for both women and men. Even so, it seems that both doctors and patients resist this fact. Maybe blaming stress feels like it belittles the problem, which is not true. The effect of stress on gut function is a real physical response triggered by our thoughts, beliefs and feelings. So, IBS is not just in our head, but the brain has a lot to do with it in a real, physical way.

- IBS treatments: proper sleep and stress reduction. Yes, 100% agreement. Poor sleep affects everything, including gut health and stress sensitivity. The article also mentions that “finding your stress management technique, whether it’s meditation, cognitive behavioral therapy or exercise is key for keeping symptoms at bay.” This is correct, but I’d add that you don’t have to choose just one stress management or release method, you can utilize multiple of them. Combining meditation with exercise for example is more effective than doing one or the other. Not to mention there are many other methods to try, too.
- Antidepressants in low doses can help. Yes, true. However, science is showing that dietary changes can be as effective as medication. For this reason experts consider diet to be a first line therapy as compared to meds.
- Low FODMAP diet is considered to be an effective approach. Yes, studies show that the low FODMAP diet helps reduce symptoms in 2/3 of cases or so. However, the article is not mentioning any risks involved with the diet. Like reduced enjoyment of eating, increased cost, food relationship changes (like food fears) and that the diet can cause stress, which is not helpful when stress is a major IBS trigger. To me, deciding on whether or not to follow the low FODMAP diet should be given thorough consideration. It shouldn’t be something automatic for every IBS patient. This even though it is one of the more natural approaches to managing IBS. Other, more simple, diet changes may be all that is needed.
- Proper hydration is key. Someone commented below the article on Instagram that they drink a lot of water, and increasing water intake doesn’t help them (this person even seemed frustrated by this advice). Both the article and the commenter are correct: drinking enough fluids is important, but if you already are drinking a lot, at least 2 liters (8 cups) a day, then drinking more is not going to help. The point is that dehydration dries out stool in the gut, predisposing us to constipation.

- Fiber is needed. It’s true that most people in the Western world don’t get enough of it, not even close. However, the article doesn’t go into any detail here, they only mention that many brands are adding fiber into their products. Fiber is critically important for gut function, and it’s important to note that there are different types of fiber that are handled differently in the gut. This is where speaking with a dietitian is helpful for making sure increasing fiber intake is done right – something the article could’ve mentioned.
- If you have persistent digestive issues, get tested. Yes, absolutely. It’s important to know your gut symptoms are not a sign of something more serious. IBS isn’t serious in the eyes of health care practitioners in that it doesn’t shorten life span, but it’s serious in a different way - it dramatically reduces quality of life. I know it can feel embarrassing to talk to a doctor about your gut function, but taking that step also brings you closer to symptom management and improving your quality of life. Remember that 10% of the global population have IBS, so it’s very common and nothing to be embarrassed about. What’s important is your health and wellbeing.
Thanks for reading! I’m glad we are talking more about IBS publicly, but much more is needed! More publications should write about IBS in an easy-to-understand way. In the meantime you can ask me. I’m here to help!
Love,
Anna-Kaisa

PS: If you have questions about this, or any other gut health or stress topic, get in touch!
PPS: Did you download my free guide “Beat Stress and Boost Your Mood” yet?
Link to the original NatGeo article here.
