If you thought the answer is “the low FODMAP diet”, you wouldn’t be the only one. Sadly, it’s not as simple as you might expect.
As a dietitian, I’ve taken care of a lot of different kinds of people with all kinds of health problems. Everyone is an individual and diet must always be individualized, but it seems that IBS is much more difficult to generalize than other health problems.
For example, if you have diabetes, you should always pay attention to everything that affects your blood sugar levels. Most often this means counting all the carbohydrates you eat, and sometimes also taking protein and fat into account. For cardiovascular disease, fat quality is something that everyone with high cholesterol needs to consider.

When it comes to IBS, there is no “one-size-fits-all” diet that works for everyone. For one, there are four different IBS types and the advice you give to someone with diarrhea is not the same if the problem is constipation instead.
While the low FODMAP diet is the most “popular” diet for IBS, in my expert opinion, the low FODMAP diet is overused and is NOT a good idea for many, if not most, people. You can read why in my two blog posts “Is the low FODMAP diet the best diet for IBS?” and “Should you try the low FODMAP diet for IBS?”. I know most other dietitians love the low FODMAP diet, but I can’t overlook all the problems that come with this diet. Yes, FODMAPs are small fibers that are easily fermented by your gut microbes and cause relatively more gas, but this happens in everyone, not just in people with IBS. The reason why you are more sensitive to them is because of visceral hypersensitivity, which is caused by IBS (this sensitivity is something I want to improve, rather than just remove foods as a bandaid solution).
So, if it’s not the low FODMAP diet, then what is the right diet for IBS?
It certainly is a highly individualized one. Here are the first five diet and food related questions you should ask yourself regardless of your IBS symptoms:
- How often do I eat?
- How big are my meals?
- How quickly do I eat?
- Do I chew my food until it’s apple sauce consistency?
- What’s my frame of mind when I eat?

I find that regular eating times, and not eating too often or too seldom, lay a foundation for a gut healthy diet. This way you are less likely to overeat or keep taxing your digestion with new food all the time. Eating too quickly results in food that is poorly chewed and a belly full of air, both of which cause bloating and indigestion. Chewing properly begins the digestive process right away and makes food more digestible. Eating when stressed, worried or angry triggers a stress response, i.e. the body’s fight-or-flight mode, which is terrible for digestion. The fight-or-flight mode is the opposite from the rest-and-digest mode. To harness the digestion-promoting rest-and-digest mode, make sure to eat when you feel calm, find a calm environment, and sit down.
Some clients of mine have found that this is all they need to keep their symptoms at bay! So, while they seem simple, these points are truly foundational and have an enormous effect on how well you digest and absorb your food.
What else for IBS?
Once the foundation is well in place, it’s important to find out if your diet is in balance, especially thinking of your individual symptoms. Balance means getting all the nutrients your body needs to be well while including food items that support easing your symptoms, and it also means that your microbiota gets all the food they need. Your gut microbes keep you well if you nourish them properly. Well-fed beneficial bacteria then send positive signals to the brain through the gut-brain axis, with health promoting effects.

A balanced diet is an optimal mix of protein, fat, and carbohydrates (including fiber), as well as vitamins, minerals and antioxidants. A plate method is a nice way of visualizing a balanced diet (see image above), but this also is a generalization that is not appropriate for everyone. It also doesn’t address fat in the diet.
What’s more, sometimes it’s not your diet that is the problem – there are situations when it doesn’t matter what you eat and your symptoms are difficult anyway. This is because IBS is caused by a problem in the way in which your gut and your brain talk to each other, and food is not exactly what causes this disruption. I talk about the gut-brain axis in a blogpost here, a great read!
Are your eating habits helping you ease IBS symptoms? Is your diet in balance?
If you are not sure, get in touch with me. During a 30-minute free gut health review I will give you the tools to build a diet that will keep your gut, and the rest of your body happy, but not only that. We’ll address your gut-brain axis also, for best results. Book your free call here.

Love,
Anna-Kaisa
PS. Don’t wait to get individualized advice for FREE! Book your call now.
PPS. Did you download my free Ebook “5 Easy Ways to Beat the Bloat” yet? These five ways are simple, yet effective in easing bloating that you can put to use right away.
The low FODMAP diet is a relatively well researched diet for IBS. Studies show that the low FODMAP diet can ease symptoms in about 2/3 of cases in varying degrees (1). But that’s just it – this diet is not a true treatment for IBS as it can only manage symptoms and not the cause of IBS. But more on that later.

The idea behind the diet is that FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides and polyols), which are naturally more difficult for the body to digest, are minimized in the diet and then brought back one FODMAP group at a time. This is because you want to only avoid those FODMAP groups that trigger symptoms – it’s not usual that all FODMAP groups are the problem. Because these fibers don’t digest well, they attract water into the intestines and are fermented (digested) by your gut microbes, both of which can cause bloating, discomfort and potentially diarrhea/constipation.
The thing is, this happens to everyone eating FODMAPs, especially in large amounts. The reason why people with IBS so often find these fibers problematic is that they have visceral hypersensitivity - they feel everything going on the intestines more strongly. Even normal things in the gut can cause bloating and pain, when normally you wouldn’t feel anything at all.
It’s important to know that FODMAPs are not bad for you. They feed the healthy gut bacteria in the large intestine, which is actually very good for your health. Avoiding FODMAPs gives the gut bacteria less food to process, which reduces their gas production and in turn gut symptoms. Unfortunately, studies have noticed that some beneficial bacteria species are reduced on the low FODMAP diet probably for this reason.
This is one reason I’m not the biggest fan of the diet. Other reasons are:
- The potential for food fears: there is a risk that you begin labeling high FODMAP foods as bad, which can lead to fear toward these foods. Fear is not helpful for gut function.
- Increased stress: the low FODMAP diet is not the easiest diet to follow. If you want to try the diet, always make sure you understand what you are doing, and even better, get guidance from an expert dietitian. Even then the diet tends to cause stress, and stress causes IBS symptoms, so following the low FODMAP diet can be counterproductive from this standpoint.
- It doesn’t treat the underlying cause: a problem in the gut-brain interaction. Perhaps, if your symptoms improve on the diet and you feel relief and reduced stress from the improvement, this can help mend the disrupted communication between the gut and the brain. But it’s not the diet change that truly did it, it’s the feelings and thoughts that followed that made the difference.
- Nutrient deficiencies: if you only cut foods out and don’t bring the right low FODMAP foods in, there is a risk of not getting enough of all the nutrients you need. Malnutrition is never supportive of gut health.
- Often there are bigger fish to fry than your diet when it comes to IBS management. If your lifestyle is not supporting your gut health, diet changes likely have a very limited impact on your symptoms. If you don’t sleep enough or if you are very stressed out for example, IBS symptoms may not be affected in any way by the low FODMAP diet.
- The low FODMAP diet asks you to avoid healthy foods, like whole grains and certain fruits and vegetables.
- Potential negative effects on your gut microbiome as mentioned above
What you eat is highly important for gut health, of course, but to me, going on the low FODMAP diet is not the best way to go, especially not as the first thing to try. Chances are I’d still recommend some individualized diet changes, but nothing too drastic to avoid the above problems. In addition, focusing on the root cause will be vital to get real IBS symptom improvement.
How do you do that? You need to think about yourself as a whole – everything that is going on in your life and your body is affecting everything else. It’s not just about food.
My best advice? Get in touch with me to see what might be the most important diet and lifestyle changes for you. Book your free session here.
Or, if you prefer to work on your own, I have the perfect self-care program for you: IBSwise. It goes over everything worthy of knowing about IBS, with many tools that you can try right away to ease your symptoms – tools that focus on mending the gut-brain communication to achieve real results. It’s an awesome program and I highly recommend it. The price is going up on 1/1/2025, so get enrolled now!
You can get started on calming the real problem behind IBS by practicing a breathing exercise like box breathing at least once daily. Go to Instagram to my account @ibsandstressdietitian and find there a short instructional video on box breathing pinned at the top of my posts. My clients are benefiting so much from practicing breathing exercises, so this tip is my gift to you.
Wishing you all the best,
Anna-Kaisa

PS. Did you get my free “5 Easy Ways to Beat the Bloat” ebook? If not, go here to get it!
References:
- Manning LP, Yao CK, Biesiekierski JR. Therapy of IBS: Is a Low FODMAP Diet the Answer? Front Psychiatry. 2020 Aug 31;11:865. doi: 10.3389/fpsyt.2020.00865. PMID: 33110411; PMCID: PMC7488954.
I had the pleasure of being hosted in an educational webinar to my fellow dietitians in Finland this past week. The topic was the connection between stress and irritable bowel syndrome. I had the opportunity to speak to over 50 of my peers about this subject that important and yet, significantly overlooked.
Many studies show the intimate connection between stress and our digestive system through the gut-brain axis. Many factors affect digestion, including the food we eat, but when stress levels are high, what we eat makes no difference – we will have gut trouble until we address the stress. Eating or not eating results in pain, bloating and either diarrhea or constipation. So yes, I can tell you that stress causes gut problems, likely also IBS, and it can certainly make it worse!
In this presentation that I gave to my fellow dietitians, I talked about the science behind stress and IBS. I went over the mechanisms through which stress affects the gut. For example, stress can cause inflammation in the gut, disrupt your gut microbiota and make the gut more sensitive to what’s happening within it, even to normal things, like a small amount of gas from bacterial fermentation of whole grains (which is good for us!).
I also went over different kinds of stress release techniques and the scientific evidence that exists for these different methods. Many different techniques are found to improve IBS symptoms, which leads me to believe that every one of us, with or without IBS, should have a stress release routine to follow every single day.
And this is not just for gut health. I believe it is impossible to have good health without stress management. It also doesn't have to be difficult, complex, or time-consuming. It can simply mean taking deep breaths before each meal, or questioning negative thoughts. Or it could be about practicing yoga and meditation regularly. Even taking a walk, taking care of your diet, sleeping well, drinking enough fluid, and spending time outdoors can do wonders to stress.
All my clients have experienced significant improvements in their gut issues when they have not only paid attention to their diet, but also started a daily stress release routine. For example, taking time to eat in peace instead of hurrying through each meal has made a big difference! Breathing exercises have also been a very central part of their stress release routines and my clients say they have been “life saving”.
If you are thinking “I don't have any stress”, I would suggest to question this, because everyone has some stress, and stress is not always felt on a mental level. Physical symptoms can be the only telltale signs of stress in your life. So, even if you don't feel like you're stressed out but are suffering from a lot of ailments, including gut issues, try stress release anyway because more than likely it will help you.
Furthermore, it will not only help your gut health, but your well-being overall.

Everything affects everything, so only adjusting your diet is not enough for true health. We need to look at every aspect of life to truly find the causes for our symptoms and the best solutions.
You can start by signing up to IBSwise and exploring the different stress release techniques I offer there, or visit my Instagram page to try the box breathing exercise that I have pinned to the top of the posts.
Any questions? Just comment below, or email me at [email protected].
Thank you for reading!
Love,
Anna-Kaisa

PS: I host free 15-minute stress release sessions on Thursdays, every other week. The next session is September 5. You can register here for the next session, and email me if you’d like a link to watch the recording from the last session.
PPS: I have lots of free stuff you can download! For example, you can get the free guide “5 Easy Ways to Beat the Bloat” here!
Earlier this month National Geographic published an article headlined “Why women are more likely to have IBS”. I love that big publications such as National Geographic are paying attention to irritable bowel syndrome, as it is so common, and as there is so much misleading information out there. Big publications could help bust some of that misinformation.

The article aimed to explore why more women than men have IBS, and to discuss some of the treatment options. Since the comments below the original Instagram post, where I first spotted the article, seemed to point out some discrepancies, I thought I’d chime in and expand on some of the unclear points. Here are some of my thoughts:
- According to Dr. Raj, a gastroenterologist, IBS is a diagnosis of exclusion – more severe illnesses with overlapping symptoms need to be ruled out before an IBS diagnosis can be made. My experience: not all doctors test for everything, like cancer and IBD. This is probably to save resources, especially in a public healthcare setting, where money is tight. However, this leads to patients feeling unsure of their diagnosis. It's one of the reasons why it's so important to be able to advocate for yourself when talking to doctors. When you know a bit about what to expect, you will feel more empowered to ask the right questions and get the help you need (one of the reasons I created IBSwise). Here’s my wish to doctors seeing patients with IBS and these kinds of gut issues: spend time explaining your decisions on testing and recommendations so that people feel heard, and can understand and accept their diagnosis and thus go for correct treatments, instead of wasting time and money looking in the wrong places.
- The reason why women are more likely to have IBS is hormones. This I can agree with. I wrote a blogpost about it.
- Another reason for women being more susceptible to IBS: sensitivity to stress. Yes, seems true. I was also glad to see stress mentioned early in the article, as this is also what I have found in my IBS research. Stress is a real culprit in IBS, for both women and men. Even so, it seems that both doctors and patients resist this fact. Maybe blaming stress feels like it belittles the problem, which is not true. The effect of stress on gut function is a real physical response triggered by our thoughts, beliefs and feelings. So, IBS is not just in our head, but the brain has a lot to do with it in a real, physical way.

- IBS treatments: proper sleep and stress reduction. Yes, 100% agreement. Poor sleep affects everything, including gut health and stress sensitivity. The article also mentions that “finding your stress management technique, whether it’s meditation, cognitive behavioral therapy or exercise is key for keeping symptoms at bay.” This is correct, but I’d add that you don’t have to choose just one stress management or release method, you can utilize multiple of them. Combining meditation with exercise for example is more effective than doing one or the other. Not to mention there are many other methods to try, too.
- Antidepressants in low doses can help. Yes, true. However, science is showing that dietary changes can be as effective as medication. For this reason experts consider diet to be a first line therapy as compared to meds.
- Low FODMAP diet is considered to be an effective approach. Yes, studies show that the low FODMAP diet helps reduce symptoms in 2/3 of cases or so. However, the article is not mentioning any risks involved with the diet. Like reduced enjoyment of eating, increased cost, food relationship changes (like food fears) and that the diet can cause stress, which is not helpful when stress is a major IBS trigger. To me, deciding on whether or not to follow the low FODMAP diet should be given thorough consideration. It shouldn’t be something automatic for every IBS patient. This even though it is one of the more natural approaches to managing IBS. Other, more simple, diet changes may be all that is needed.
- Proper hydration is key. Someone commented below the article on Instagram that they drink a lot of water, and increasing water intake doesn’t help them (this person even seemed frustrated by this advice). Both the article and the commenter are correct: drinking enough fluids is important, but if you already are drinking a lot, at least 2 liters (8 cups) a day, then drinking more is not going to help. The point is that dehydration dries out stool in the gut, predisposing us to constipation.

- Fiber is needed. It’s true that most people in the Western world don’t get enough of it, not even close. However, the article doesn’t go into any detail here, they only mention that many brands are adding fiber into their products. Fiber is critically important for gut function, and it’s important to note that there are different types of fiber that are handled differently in the gut. This is where speaking with a dietitian is helpful for making sure increasing fiber intake is done right – something the article could’ve mentioned.
- If you have persistent digestive issues, get tested. Yes, absolutely. It’s important to know your gut symptoms are not a sign of something more serious. IBS isn’t serious in the eyes of health care practitioners in that it doesn’t shorten life span, but it’s serious in a different way - it dramatically reduces quality of life. I know it can feel embarrassing to talk to a doctor about your gut function, but taking that step also brings you closer to symptom management and improving your quality of life. Remember that 10% of the global population have IBS, so it’s very common and nothing to be embarrassed about. What’s important is your health and wellbeing.
Thanks for reading! I’m glad we are talking more about IBS publicly, but much more is needed! More publications should write about IBS in an easy-to-understand way. In the meantime you can ask me. I’m here to help!
Love,
Anna-Kaisa

PS: If you have questions about this, or any other gut health or stress topic, get in touch!
PPS: Did you download my free guide “Beat Stress and Boost Your Mood” yet?
Link to the original NatGeo article here.
Have you noticed that your gut functions differently depending on where you are in your cycle? That every time you are about to have your period, your gut gets messed up, or your already loose stools become worse?
You are not imagining it – female hormones do affect the gut, especially through pain sensitivity, how fast the gut contents move (motility), and indirectly through greater stress sensitivity (1-4). Female hormones could explain why women tend to have more IBS than men in general, and more IBS-C than men (1,2). In this article, I briefly go over what this means in terms of gut symptoms.
Menstrual cycle
First, let’s briefly discuss the menstrual cycle. There are three phases:
| Phase | Days | Estrogen and progesterone | Gut impact |
| Menstruation phase | 1-7 | Both are low | Faster motility, higher risk of diarrhea, urgency Increased pain sensitivity |
| Follicular phase | 8-14 (until ovulation) | Estrogen: Increases until peaks at ovulation Progesterone: low | Slower motility |
| Luteal phase | 15-28 | Estrogen: high, drops quickly Progesterone: high | Slower motility |
Female hormones and the gut
Now, let’s dive into how female hormones can change how the gut functions.
Motility
Very simply put (I discuss this subject in more detail in my IBSwise course), estrogen affects the gut by lengthening gut transit time, which means that gut contents move slower through the intestines. When estrogen levels are high, gut moves slower, and when estrogen levels drop, gut motility increases. This is probably why women tend to be more prone to IBS-C, and have constipation especially during follicular and early luteal phases, and higher chance of diarrhea around menstruation. During pregnancy, estrogen levels are high, which could at least partially explain why constipation is so common in pregnant women, especially during the third trimester. (1,2)
On the other hand, progesterone’s effect on gut motility is not as clear, as it affects serotonin mechanisms also, but the overall effect seems to be similar to estrogen: higher levels are associated with slower gut movements (1).
Pain sensitivity
It’s unclear how estrogen affects pain sensitivity, but it looks like changes in estrogen predispose to pain, such as a few days after ovulation when estrogen levels drop quickly (6). Pain sensitivity has also been found to be higher around menstruation when there is an increased number of serotonin receptors due to low estrogen, which leads to detecting pain and sensations more easily. Estrogen affects inflammatory pathways as well, which can lead to higher sensitivity – in IBS it has been noted that the number of a certain estrogen receptor is often high, which increases inflammation and therefore pain sensitivity (1,3,4).

Stress
Another mechanism that can increase gut symptoms in women is that women are naturally more reactive to stress than men. Female sex hormones have been connected to HPA-axis activity, and to a higher limbic system activity (1-3). This all lowers the threshold for a stress response to be triggered in the body, which leads to gut issues, especially in IBS.
Birth control?
What about women on birth control? According to Dr. Liao (5), birth control that allows for menstruation doesn’t protect from hormonal gut changes, but ones that skip menstruation could. Discuss with your doctor if you feel that at different phases of your cycle you experience difficult symptoms, whether it’s constipation during follicular and early luteal phase, or diarrhea and pain around menstruation phase. Still, even though female hormones seem to affect gut symptoms, data doesn’t support utilizing hormone therapies for women with IBS (3).

What can you do about it?
If your gut behaves differently during different phases of the menstrual cycle, it’s nice to know it is caused by your hormones. While I don’t recommend observing gut symptoms too closely, knowing when you are more likely to have diarrhea vs constipation could help you anticipate these changes.
Perhaps you can prepare a bit, also – if you are often constipated outside of menstruation, you could increase the amount of fiber you eat at that time of the month, whereas if you experience diarrhea during and close to menstruation, you could utilize soluble fiber from chia seeds, flaxseed and oatmeal. Additionally, focusing on anti-inflammatory foods during menstruation may be useful, like eating lots of colorful fruits and vegetables, and omega-3 rich foods, like walnuts, hempseed, and salmon, although these are important foods to eat every day.
So, female hormones and gut function are connected. Knowing how is useful, as you won’t be surprised by the changes, nor will there be a need to be worried. And you can make better food choices according to your cycle too.
Have a great summer!
Love,
Anna-Kaisa from AKWise

PS: Check out all the free giveaways on my home page!
References
- Meleine M, Matricon J. Gender-related differences in irritable bowel syndrome: potential mechanisms of sex hormones. World J Gastroenterol. 2014 Jun 14;20(22):6725-43. doi: 10.3748/wjg.v20.i22.6725. PMID: 24944465; PMCID: PMC4051914. 3
- Mulak A, Taché Y, Larauche M. Sex hormones in the modulation of irritable bowel syndrome. World J Gastroenterol. 2014 Mar 14;20(10):2433-48. doi: 10.3748/wjg.v20.i10.2433. PMID: 24627581; PMCID: PMC3949254. 4
- Pati GK, Kar C, Narayan J, Uthansingh K, Behera M, Sahu MK, Mishra D, Singh A. Irritable Bowel Syndrome and the Menstrual Cycle. Cureus. 2021 Jan 14;13(1):e12692. doi: 10.7759/cureus.12692. PMID: 33614302; PMCID: PMC7883586. 5
- Chen C, Gong X, Yang X, Shang X, Du Q, Liao Q, Xie R, Chen Y, Xu J. The roles of estrogen and estrogen receptors in gastrointestinal disease. Oncol Lett. 2019 Dec;18(6):5673-5680. doi: 10.3892/ol.2019.10983. Epub 2019 Oct 11. PMID: 31788039; PMCID: PMC6865762.
- Liao, S. Do Your Hormones Affect IBS? WebMD. https://www.webmd.com/ibs/hormones-ibs. Accessed 6/16/2024
- Athnaiel O, Cantillo S, Paredes S, Knezevic NN. The Role of Sex Hormones in Pain-Related Conditions. Int J Mol Sci. 2023 Jan 18;24(3):1866. doi: 10.3390/ijms24031866. PMID: 36768188; PMCID: PMC9915903.
Did you know that irritable bowel syndrome is now being classified as a disorder of gut-brain interaction? This is a big deal, because this classification also suggests a way to reverse IBS – by fixing this disordered gut-brain interaction!
But let’s back up a little – what is gut-brain interaction anyway? Well, simply put, our gut and our brain communicate with each other constantly: the gut is sending signals about what is going in the gut and its contents and the brain is talking to the gut about our environment, such as of safety or danger.
In a disordered gut-brain communication, the gut is telling the brain there are problems when there aren’t necessarily any, and the brain might be telling the gut that we are in danger when we are not. All of this might even become a vicious cycle, in which the gut and the brain feed off of each other and make everything worse.
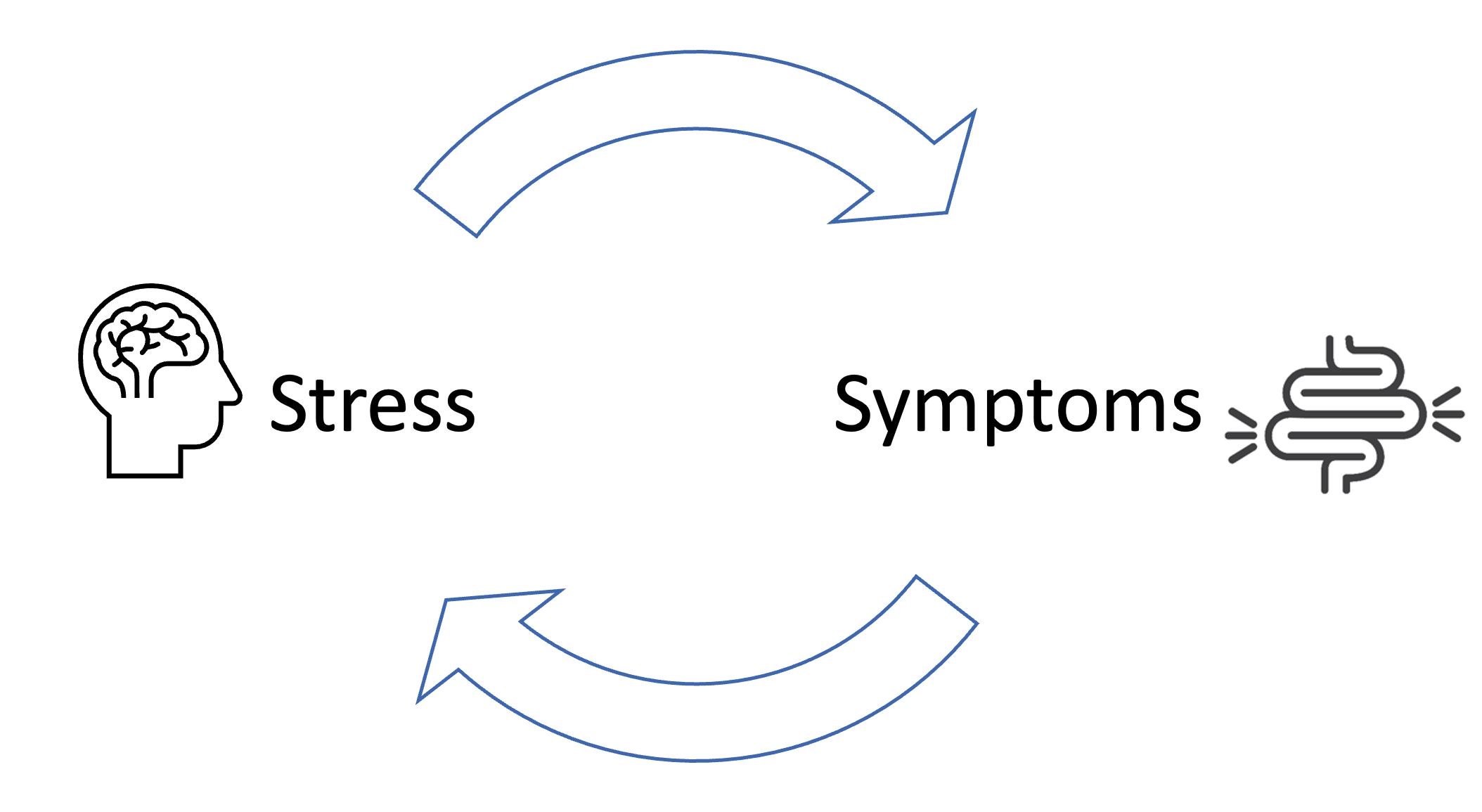
What causes the gut-brain connection to go haywire? Sometimes a gut infection or antibiotics may trigger persistent gut symptoms probably because of inflammation and gut microbiota changes (1,2), but more importantly, all other signs point to stress. Having extensively studied and researched the mechanisms of IBS (such as visceral hypersensitivity, gut immune function changes, increased gut permeability and gut microbiota dysbiosis), all of them can be caused by stress (3). And stress is what causes the brain to send distress signals to the gut.
For example, most of us have experienced a time when we were really nervous about something, like giving a presentation or having a sports competition, that lead to abdominal pain and maybe diarrhea. I certainly can remember many instances! What happens, is that the brain prepares the body for a dangerous situation, which triggers a stress response in the body (an important survival mechanism!), to which the gut responds by becoming hypersensitive (pain) and removing its contents (diarrhea), or not moving its contents (constipation) so that the body could be better prepared to fight or flee (4).
Usually when the event is over, the body returns to rest-and-digest mode and digestion goes back to normal. However, in IBS, a stress response has gotten stuck or triggers more easily leading to more persistent gut symptoms (3,5).
How then do we calm the disordered gut-brain interaction? The key is to switch the brain and the body to the rest-and-digest mode. The vagus nerve plays a big part in this and by stimulating this nerve we can restore proper communications between the gut and the brain.

And there are many ways to do this! My IBSwise course discusses most of them and provides opportunities to try them, too – I heartily recommend checking it out.
One thing you can do right away: take deep diaphragmatic (belly) breaths before each meal and any time you are feeling stressed out – this is a very simple way to calm and relax the body and boost digestion. Also try yoga and meditation practices, other breathing exercises and spending more time in nature etc. I also talk about all of these and many others on IBSwise.
Thanks for reading! There is so much you can do for your gut health that is free and doesn’t require medication or supplements! Get in touch if you have any questions.
Love,
Anna-Kaisa

References
- Lupu VV, Ghiciuc CM, Stefanescu G, Mihai CM, Popp A, Sasaran MO, Bozomitu L, Starcea IM, Adam Raileanu A, Lupu A. Emerging role of the gut microbiome in post-infectious irritable bowel syndrome: A literature review. World J Gastroenterol. 2023 Jun 7;29(21):3241-3256. doi: 10.3748/wjg.v29.i21.3241. PMID: 37377581; PMCID: PMC10292139.
- Mamieva Z, Poluektova E, Svistushkin V, Sobolev V, Shifrin O, Guarner F, Ivashkin V. Antibiotics, gut microbiota, and irritable bowel syndrome: What are the relations? World J Gastroenterol. 2022 Mar 28;28(12):1204-1219. doi: 10.3748/wjg.v28.i12.1204. PMID: 35431513; PMCID: PMC8968486.
- Qin HY, Cheng CW, Tang XD, Bian ZX. Impact of psychological stress on irritable bowel syndrome. World J Gastroenterol. 2014 Oct 21;20(39):14126-31. doi: 10.3748/wjg.v20.i39.14126. PMID: 25339801; PMCID: PMC4202343.
- Stress Effects. The American Institute of Stress. https://www.stress.org/stress-effects. Accessed 24/2/2024.
- Punkkinen et al. Suoli-aivoakseli vai aivo-suoliakseli – hoitokeinoja toiminnallisiin vatsavaivoihin. Review. Lääketieteellinen aikakauskirja Duodecim. 2023;139(22):1831-9
