Have you noticed that your gut functions differently depending on where you are in your cycle? That every time you are about to have your period, your gut gets messed up, or your already loose stools become worse?
You are not imagining it – female hormones do affect the gut, especially through pain sensitivity, how fast the gut contents move (motility), and indirectly through greater stress sensitivity (1-4). Female hormones could explain why women tend to have more IBS than men in general, and more IBS-C than men (1,2). In this article, I briefly go over what this means in terms of gut symptoms.
Menstrual cycle
First, let’s briefly discuss the menstrual cycle. There are three phases:
| Phase | Days | Estrogen and progesterone | Gut impact |
| Menstruation phase | 1-7 | Both are low | Faster motility, higher risk of diarrhea, urgency Increased pain sensitivity |
| Follicular phase | 8-14 (until ovulation) | Estrogen: Increases until peaks at ovulation Progesterone: low | Slower motility |
| Luteal phase | 15-28 | Estrogen: high, drops quickly Progesterone: high | Slower motility |
Female hormones and the gut
Now, let’s dive into how female hormones can change how the gut functions.
Motility
Very simply put (I discuss this subject in more detail in my IBSwise course), estrogen affects the gut by lengthening gut transit time, which means that gut contents move slower through the intestines. When estrogen levels are high, gut moves slower, and when estrogen levels drop, gut motility increases. This is probably why women tend to be more prone to IBS-C, and have constipation especially during follicular and early luteal phases, and higher chance of diarrhea around menstruation. During pregnancy, estrogen levels are high, which could at least partially explain why constipation is so common in pregnant women, especially during the third trimester. (1,2)
On the other hand, progesterone’s effect on gut motility is not as clear, as it affects serotonin mechanisms also, but the overall effect seems to be similar to estrogen: higher levels are associated with slower gut movements (1).
Pain sensitivity
It’s unclear how estrogen affects pain sensitivity, but it looks like changes in estrogen predispose to pain, such as a few days after ovulation when estrogen levels drop quickly (6). Pain sensitivity has also been found to be higher around menstruation when there is an increased number of serotonin receptors due to low estrogen, which leads to detecting pain and sensations more easily. Estrogen affects inflammatory pathways as well, which can lead to higher sensitivity – in IBS it has been noted that the number of a certain estrogen receptor is often high, which increases inflammation and therefore pain sensitivity (1,3,4).

Stress
Another mechanism that can increase gut symptoms in women is that women are naturally more reactive to stress than men. Female sex hormones have been connected to HPA-axis activity, and to a higher limbic system activity (1-3). This all lowers the threshold for a stress response to be triggered in the body, which leads to gut issues, especially in IBS.
Birth control?
What about women on birth control? According to Dr. Liao (5), birth control that allows for menstruation doesn’t protect from hormonal gut changes, but ones that skip menstruation could. Discuss with your doctor if you feel that at different phases of your cycle you experience difficult symptoms, whether it’s constipation during follicular and early luteal phase, or diarrhea and pain around menstruation phase. Still, even though female hormones seem to affect gut symptoms, data doesn’t support utilizing hormone therapies for women with IBS (3).

What can you do about it?
If your gut behaves differently during different phases of the menstrual cycle, it’s nice to know it is caused by your hormones. While I don’t recommend observing gut symptoms too closely, knowing when you are more likely to have diarrhea vs constipation could help you anticipate these changes.
Perhaps you can prepare a bit, also – if you are often constipated outside of menstruation, you could increase the amount of fiber you eat at that time of the month, whereas if you experience diarrhea during and close to menstruation, you could utilize soluble fiber from chia seeds, flaxseed and oatmeal. Additionally, focusing on anti-inflammatory foods during menstruation may be useful, like eating lots of colorful fruits and vegetables, and omega-3 rich foods, like walnuts, hempseed, and salmon, although these are important foods to eat every day.
So, female hormones and gut function are connected. Knowing how is useful, as you won’t be surprised by the changes, nor will there be a need to be worried. And you can make better food choices according to your cycle too.
Have a great summer!
Love,
Anna-Kaisa from AKWise

PS: Check out all the free giveaways on my home page!
References
- Meleine M, Matricon J. Gender-related differences in irritable bowel syndrome: potential mechanisms of sex hormones. World J Gastroenterol. 2014 Jun 14;20(22):6725-43. doi: 10.3748/wjg.v20.i22.6725. PMID: 24944465; PMCID: PMC4051914. 3
- Mulak A, Taché Y, Larauche M. Sex hormones in the modulation of irritable bowel syndrome. World J Gastroenterol. 2014 Mar 14;20(10):2433-48. doi: 10.3748/wjg.v20.i10.2433. PMID: 24627581; PMCID: PMC3949254. 4
- Pati GK, Kar C, Narayan J, Uthansingh K, Behera M, Sahu MK, Mishra D, Singh A. Irritable Bowel Syndrome and the Menstrual Cycle. Cureus. 2021 Jan 14;13(1):e12692. doi: 10.7759/cureus.12692. PMID: 33614302; PMCID: PMC7883586. 5
- Chen C, Gong X, Yang X, Shang X, Du Q, Liao Q, Xie R, Chen Y, Xu J. The roles of estrogen and estrogen receptors in gastrointestinal disease. Oncol Lett. 2019 Dec;18(6):5673-5680. doi: 10.3892/ol.2019.10983. Epub 2019 Oct 11. PMID: 31788039; PMCID: PMC6865762.
- Liao, S. Do Your Hormones Affect IBS? WebMD. https://www.webmd.com/ibs/hormones-ibs. Accessed 6/16/2024
- Athnaiel O, Cantillo S, Paredes S, Knezevic NN. The Role of Sex Hormones in Pain-Related Conditions. Int J Mol Sci. 2023 Jan 18;24(3):1866. doi: 10.3390/ijms24031866. PMID: 36768188; PMCID: PMC9915903.
Most people don’t feel great after eating a large amount of sugar in one form or the other, I know I’ve been there many times! On top of feeling off or crashing from blood sugar swings, some may even get a stomachache, diarrhea or become bloated - your typical IBS symptoms. We know that carbohydrates, including sugars, affect the gut, and in this post I will briefly discuss what is known specifically about the effect of sugar (excluding lactose in dairy) on gut function. Is it something we should avoid eating altogether?

To lay the foundation, sugar is simple carbohydrate, and there are actually many types of sugar. What is important to know is that all carbohydrate (starch) must be turned into sugar before it can be absorbed, and more specifically, into single sugar units called monosaccharides. Even two sugar molecules together, like sucrose in table sugar is too large to be absorbed. So, despite what we may have heard, this also means that sugar is not in and of itself bad for us AND all the cells in our body prefer to be fueled by the monosaccharide glucose. It’s more that high sugar foods tend to be highly processed and poor in other nutrients, like vitamins and minerals that doesn’t promote general health.
Fructose is a monosaccharide sugar found in fruit and processed foods. Fructose is also considered a FODMAP – a highly fermentable sugar that in large amounts can naturally cause gut symptoms. This is because fructose absorbs relatively poorly from the intestines as compared to glucose, and if the amount of fructose that was eaten is high enough, it can travel all the way to the large intestine where our gut microbes feast on it, causing gas formation, bloating and diarrhea. (1)

Another way in which fructose can trigger gut problems is that when there is enough of fructose particles together in the gut, they attract water to themselves (happens with any particles, not just fructose). This can lead to a fluid buildup in the intestine quickening it’s movement and volume, which can then lead to a fast exit, and discomfort. However, if fructose is together with glucose, it absorbs better and is likely to not cause any gut issues. (1)
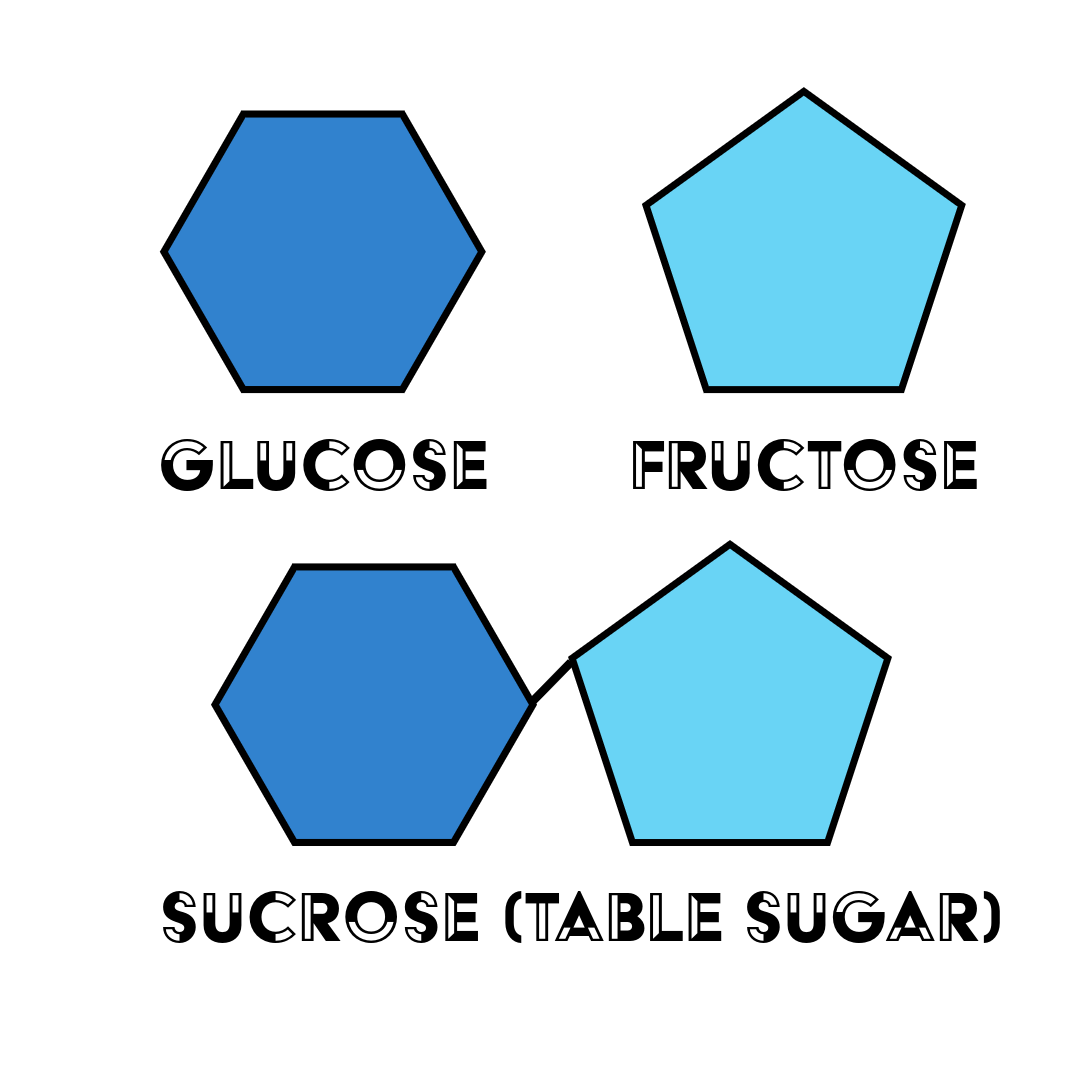
Table sugar, or sucrose, is an example of a disaccharide in which a glucose and a fructose molecule are stuck together. High-fructose corn syrup, on the other hand, is a sweetener that has more fructose than glucose in it, as is fruit juice and honey. It is this excess of fructose as compared to glucose that can pose a problem when eaten in a large enough amount. And this is not just with people with IBS, but everyone – in fact, when fructose malabsorption is tested, people with IBS are not different from healthy people. (1)
You might then wonder if adding some glucose to foods that have a lot of fructose would help the fructose absorb better and thus prevent gut symptoms? Scientists have been wondering the same and while theoretically this would make sense, scientific studies haven’t been able to show this to be helpful in reducing gut symptoms (2).
But what about high sugar foods that don’t have more fructose than glucose in it? Could this kind of sugar also cause gut trouble?
The short answer is yes, it could.
In theory, sucrose and especially glucose are sugars that absorb quickly and quite completely in the small intestine so that they shouldn’t really end up in the large intestine to be fermented by our gut microbes and cause problems.
But one reason sucrose, or table sugar, could lead to gut symptoms is a genetic disorder called sucrase-isomaltase deficiency, in which the enzyme that breaks down sucrose is missing or not working well which lets this sugar stay in the gut to attract water and travel into the large intestine to be fermented. This is very rare, however. But, if you always have gut symptoms after eating sugary food, and the low FODMAP diet hasn’t helped, and especially if you have had issues since childhood, experts suggest checking for sucrase-isomaltase deficiency. (3)
Another, and perhaps more likely, theory is that it is overloading the gut with sugar that triggers problems: the amount of sugar is bigger than what the intestine can absorb, attracting water to itself, moving too quickly through the small intestine, and becoming fermented in the large intestine.

A study investigating a diet low in starch and sucrose found that this diet helped reduce gut symptoms – as for the mechanism, they suggested sugar overload also, and also that the gut microbiota become improved on a lower sugar and starch diet (4). This could also be due to the fact that when we eat less sugar, we might eat more foods that positively nourish the microbiota. However, what is important, is that the authors of the study remind us that gut health is a sum of all the dietary and lifestyle choices we make, rather than depending on one or even a few foods or nutrients in our diet.
In the end, it all comes down to moderation – large amounts of anything can cause gut symptoms.
So no, you don’t have to stop eating sugar to keep your gut healthy. In addition to moderation, something also to consider is how you eat your sweets - do you eat them into an empty stomach or as a dessert? This changes how you digest the sugars in the food (I suggest you eat your sweets as a dessert).
And what else are you eating? Is your diet in balance? Is your lifestyle in balance? What can you do to bring more balance into your life so that you can enjoy a moderate amount of sugar without gut or health issues? If you are not sure, here’s a lifestyle checklist you can download to spot more easily what those changes could be.
Thank you for reading! I’d love to hear your thoughts and also your requests for future blog posts.
Love,
Anna-Kaisa

PS: I created an IBS course called IBSwise to help people with gut issues to achieve IBS freedom! But if you’d like a more individualized approach, book a call with me to see how I can help you improve your digestive health without restrictive diets and giving up foods or nutrients.
References
- Fernández-Bañares F. Carbohydrate Maldigestion and Intolerance. Nutrients. 2022 May 4;14(9):1923. doi: 10.3390/nu14091923. PMID: 35565890; PMCID: PMC9099680.
- Tuck, C.J., et al., Adding glucose to food and solutions to enhance fructose absorption is not effective in preventing fructose-induced functional gastrointestinal symptoms: randomized controlled trials in patients with fructose malabsorption. Journal of Human Nutrition and Dietetics, 2017. 30(1): p. 73-82.
- Foley A, Halmos EP, Husein DM, et al Adult sucrase-isomaltase deficiency masquerading as IBS Gut 2022;71:1237-1238.
- Nilholm C, Roth B, Ohlsson B. A Dietary Intervention with Reduction of Starch and Sucrose Leads to Reduced Gastrointestinal and Extra-Intestinal Symptoms in IBS Patients. Nutrients. 2019 Jul 20;11(7):1662. doi: 10.3390/nu11071662. PMID: 31330810; PMCID: PMC6682926.
Did you know that irritable bowel syndrome is now being classified as a disorder of gut-brain interaction? This is a big deal, because this classification also suggests a way to reverse IBS – by fixing this disordered gut-brain interaction!
But let’s back up a little – what is gut-brain interaction anyway? Well, simply put, our gut and our brain communicate with each other constantly: the gut is sending signals about what is going in the gut and its contents and the brain is talking to the gut about our environment, such as of safety or danger.
In a disordered gut-brain communication, the gut is telling the brain there are problems when there aren’t necessarily any, and the brain might be telling the gut that we are in danger when we are not. All of this might even become a vicious cycle, in which the gut and the brain feed off of each other and make everything worse.
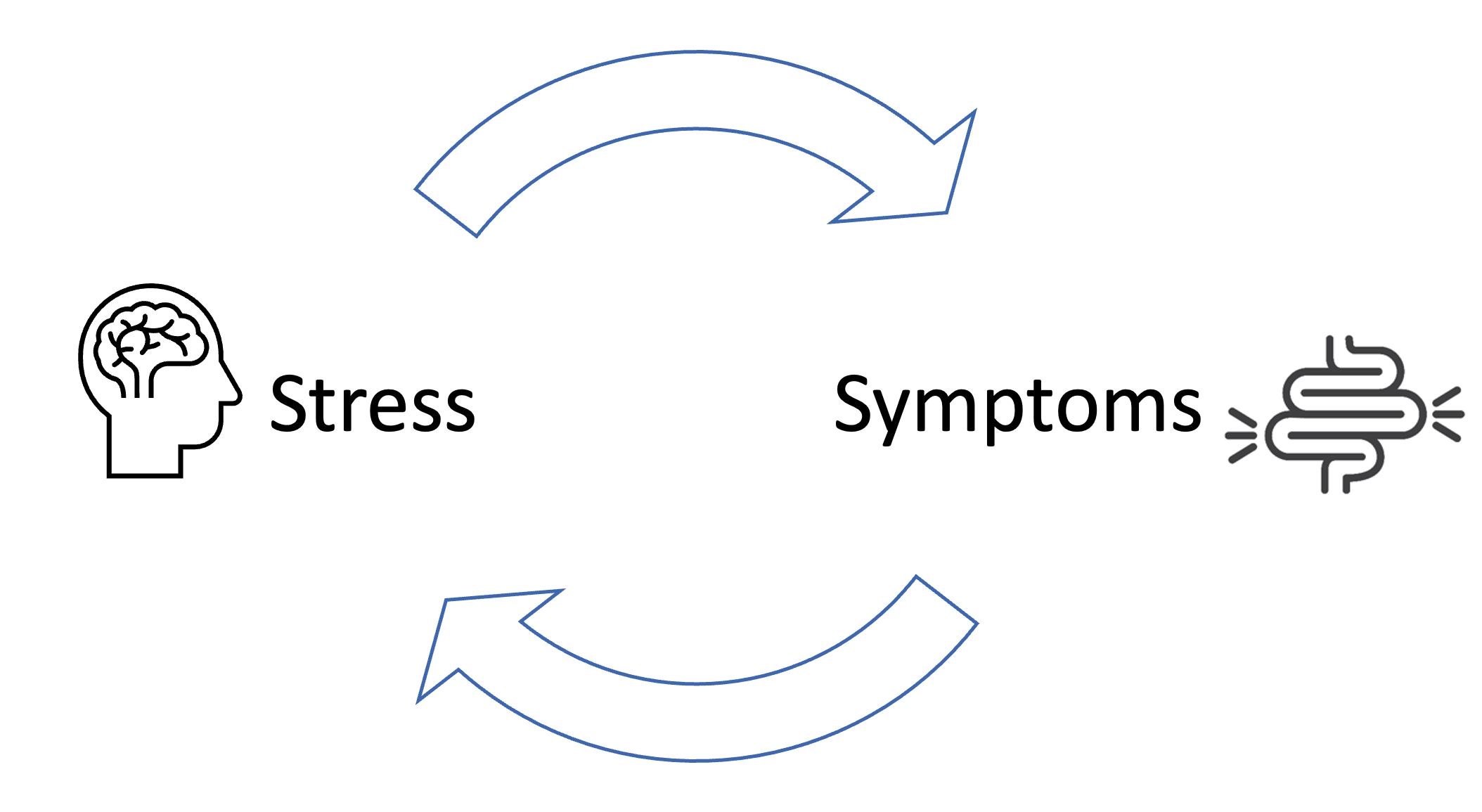
What causes the gut-brain connection to go haywire? Sometimes a gut infection or antibiotics may trigger persistent gut symptoms probably because of inflammation and gut microbiota changes (1,2), but more importantly, all other signs point to stress. Having extensively studied and researched the mechanisms of IBS (such as visceral hypersensitivity, gut immune function changes, increased gut permeability and gut microbiota dysbiosis), all of them can be caused by stress (3). And stress is what causes the brain to send distress signals to the gut.
For example, most of us have experienced a time when we were really nervous about something, like giving a presentation or having a sports competition, that lead to abdominal pain and maybe diarrhea. I certainly can remember many instances! What happens, is that the brain prepares the body for a dangerous situation, which triggers a stress response in the body (an important survival mechanism!), to which the gut responds by becoming hypersensitive (pain) and removing its contents (diarrhea), or not moving its contents (constipation) so that the body could be better prepared to fight or flee (4).
Usually when the event is over, the body returns to rest-and-digest mode and digestion goes back to normal. However, in IBS, a stress response has gotten stuck or triggers more easily leading to more persistent gut symptoms (3,5).
How then do we calm the disordered gut-brain interaction? The key is to switch the brain and the body to the rest-and-digest mode. The vagus nerve plays a big part in this and by stimulating this nerve we can restore proper communications between the gut and the brain.

And there are many ways to do this! My IBSwise course discusses most of them and provides opportunities to try them, too – I heartily recommend checking it out.
One thing you can do right away: take deep diaphragmatic (belly) breaths before each meal and any time you are feeling stressed out – this is a very simple way to calm and relax the body and boost digestion. Also try yoga and meditation practices, other breathing exercises and spending more time in nature etc. I also talk about all of these and many others on IBSwise.
Thanks for reading! There is so much you can do for your gut health that is free and doesn’t require medication or supplements! Get in touch if you have any questions.
Love,
Anna-Kaisa

References
- Lupu VV, Ghiciuc CM, Stefanescu G, Mihai CM, Popp A, Sasaran MO, Bozomitu L, Starcea IM, Adam Raileanu A, Lupu A. Emerging role of the gut microbiome in post-infectious irritable bowel syndrome: A literature review. World J Gastroenterol. 2023 Jun 7;29(21):3241-3256. doi: 10.3748/wjg.v29.i21.3241. PMID: 37377581; PMCID: PMC10292139.
- Mamieva Z, Poluektova E, Svistushkin V, Sobolev V, Shifrin O, Guarner F, Ivashkin V. Antibiotics, gut microbiota, and irritable bowel syndrome: What are the relations? World J Gastroenterol. 2022 Mar 28;28(12):1204-1219. doi: 10.3748/wjg.v28.i12.1204. PMID: 35431513; PMCID: PMC8968486.
- Qin HY, Cheng CW, Tang XD, Bian ZX. Impact of psychological stress on irritable bowel syndrome. World J Gastroenterol. 2014 Oct 21;20(39):14126-31. doi: 10.3748/wjg.v20.i39.14126. PMID: 25339801; PMCID: PMC4202343.
- Stress Effects. The American Institute of Stress. https://www.stress.org/stress-effects. Accessed 24/2/2024.
- Punkkinen et al. Suoli-aivoakseli vai aivo-suoliakseli – hoitokeinoja toiminnallisiin vatsavaivoihin. Review. Lääketieteellinen aikakauskirja Duodecim. 2023;139(22):1831-9
