Most people don’t feel great after eating a large amount of sugar in one form or the other, I know I’ve been there many times! On top of feeling off or crashing from blood sugar swings, some may even get a stomachache, diarrhea or become bloated - your typical IBS symptoms. We know that carbohydrates, including sugars, affect the gut, and in this post I will briefly discuss what is known specifically about the effect of sugar (excluding lactose in dairy) on gut function. Is it something we should avoid eating altogether?

To lay the foundation, sugar is simple carbohydrate, and there are actually many types of sugar. What is important to know is that all carbohydrate (starch) must be turned into sugar before it can be absorbed, and more specifically, into single sugar units called monosaccharides. Even two sugar molecules together, like sucrose in table sugar is too large to be absorbed. So, despite what we may have heard, this also means that sugar is not in and of itself bad for us AND all the cells in our body prefer to be fueled by the monosaccharide glucose. It’s more that high sugar foods tend to be highly processed and poor in other nutrients, like vitamins and minerals that doesn’t promote general health.
Fructose is a monosaccharide sugar found in fruit and processed foods. Fructose is also considered a FODMAP – a highly fermentable sugar that in large amounts can naturally cause gut symptoms. This is because fructose absorbs relatively poorly from the intestines as compared to glucose, and if the amount of fructose that was eaten is high enough, it can travel all the way to the large intestine where our gut microbes feast on it, causing gas formation, bloating and diarrhea. (1)

Another way in which fructose can trigger gut problems is that when there is enough of fructose particles together in the gut, they attract water to themselves (happens with any particles, not just fructose). This can lead to a fluid buildup in the intestine quickening it’s movement and volume, which can then lead to a fast exit, and discomfort. However, if fructose is together with glucose, it absorbs better and is likely to not cause any gut issues. (1)
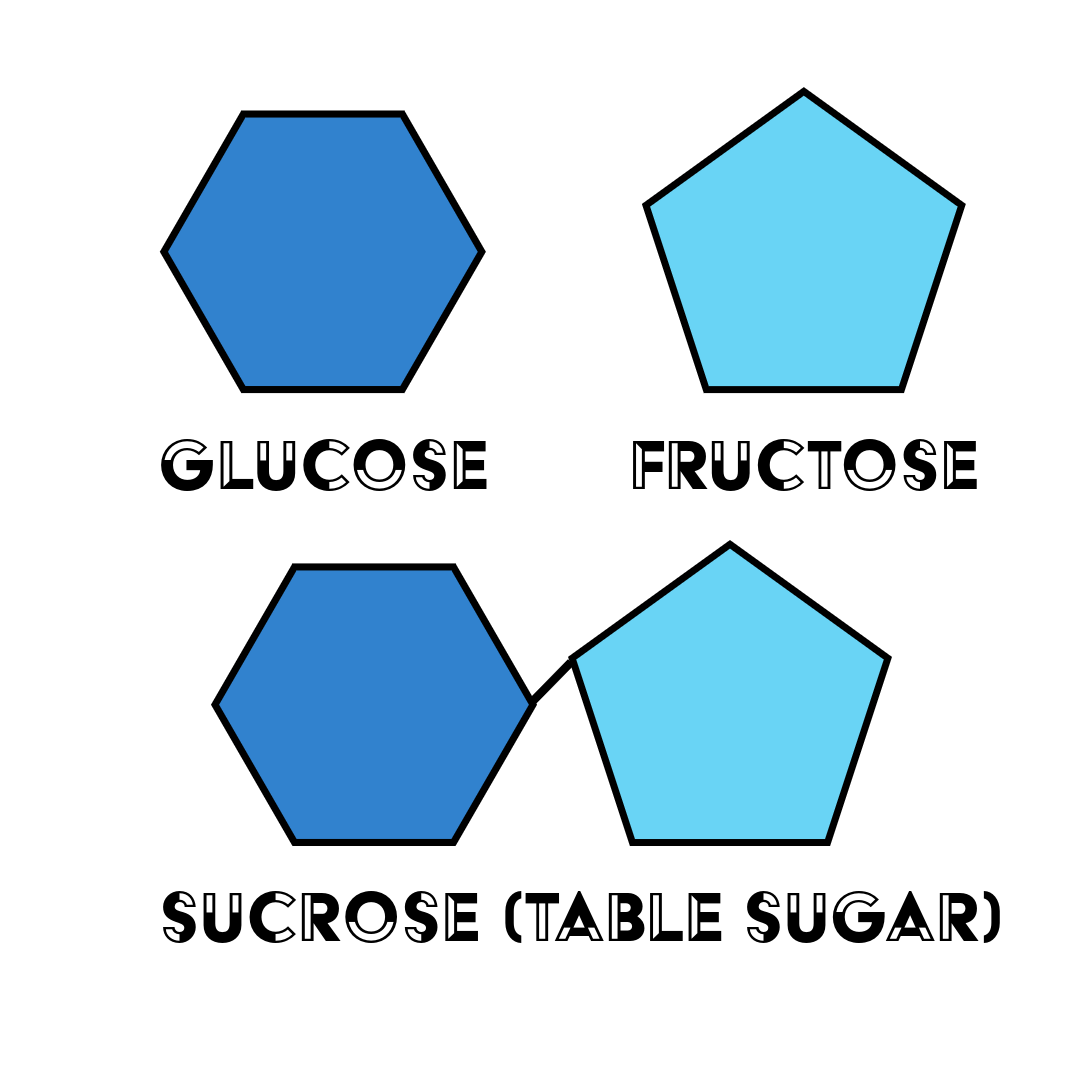
Table sugar, or sucrose, is an example of a disaccharide in which a glucose and a fructose molecule are stuck together. High-fructose corn syrup, on the other hand, is a sweetener that has more fructose than glucose in it, as is fruit juice and honey. It is this excess of fructose as compared to glucose that can pose a problem when eaten in a large enough amount. And this is not just with people with IBS, but everyone – in fact, when fructose malabsorption is tested, people with IBS are not different from healthy people. (1)
You might then wonder if adding some glucose to foods that have a lot of fructose would help the fructose absorb better and thus prevent gut symptoms? Scientists have been wondering the same and while theoretically this would make sense, scientific studies haven’t been able to show this to be helpful in reducing gut symptoms (2).
But what about high sugar foods that don’t have more fructose than glucose in it? Could this kind of sugar also cause gut trouble?
The short answer is yes, it could.
In theory, sucrose and especially glucose are sugars that absorb quickly and quite completely in the small intestine so that they shouldn’t really end up in the large intestine to be fermented by our gut microbes and cause problems.
But one reason sucrose, or table sugar, could lead to gut symptoms is a genetic disorder called sucrase-isomaltase deficiency, in which the enzyme that breaks down sucrose is missing or not working well which lets this sugar stay in the gut to attract water and travel into the large intestine to be fermented. This is very rare, however. But, if you always have gut symptoms after eating sugary food, and the low FODMAP diet hasn’t helped, and especially if you have had issues since childhood, experts suggest checking for sucrase-isomaltase deficiency. (3)
Another, and perhaps more likely, theory is that it is overloading the gut with sugar that triggers problems: the amount of sugar is bigger than what the intestine can absorb, attracting water to itself, moving too quickly through the small intestine, and becoming fermented in the large intestine.

A study investigating a diet low in starch and sucrose found that this diet helped reduce gut symptoms – as for the mechanism, they suggested sugar overload also, and also that the gut microbiota become improved on a lower sugar and starch diet (4). This could also be due to the fact that when we eat less sugar, we might eat more foods that positively nourish the microbiota. However, what is important, is that the authors of the study remind us that gut health is a sum of all the dietary and lifestyle choices we make, rather than depending on one or even a few foods or nutrients in our diet.
In the end, it all comes down to moderation – large amounts of anything can cause gut symptoms.
So no, you don’t have to stop eating sugar to keep your gut healthy. In addition to moderation, something also to consider is how you eat your sweets - do you eat them into an empty stomach or as a dessert? This changes how you digest the sugars in the food (I suggest you eat your sweets as a dessert).
And what else are you eating? Is your diet in balance? Is your lifestyle in balance? What can you do to bring more balance into your life so that you can enjoy a moderate amount of sugar without gut or health issues? If you are not sure, here’s a lifestyle checklist you can download to spot more easily what those changes could be.
Thank you for reading! I’d love to hear your thoughts and also your requests for future blog posts.
Love,
Anna-Kaisa

PS: I created an IBS course called IBSwise to help people with gut issues to achieve IBS freedom! But if you’d like a more individualized approach, book a call with me to see how I can help you improve your digestive health without restrictive diets and giving up foods or nutrients.
References
- Fernández-Bañares F. Carbohydrate Maldigestion and Intolerance. Nutrients. 2022 May 4;14(9):1923. doi: 10.3390/nu14091923. PMID: 35565890; PMCID: PMC9099680.
- Tuck, C.J., et al., Adding glucose to food and solutions to enhance fructose absorption is not effective in preventing fructose-induced functional gastrointestinal symptoms: randomized controlled trials in patients with fructose malabsorption. Journal of Human Nutrition and Dietetics, 2017. 30(1): p. 73-82.
- Foley A, Halmos EP, Husein DM, et al Adult sucrase-isomaltase deficiency masquerading as IBS Gut 2022;71:1237-1238.
- Nilholm C, Roth B, Ohlsson B. A Dietary Intervention with Reduction of Starch and Sucrose Leads to Reduced Gastrointestinal and Extra-Intestinal Symptoms in IBS Patients. Nutrients. 2019 Jul 20;11(7):1662. doi: 10.3390/nu11071662. PMID: 31330810; PMCID: PMC6682926.

